Review Article | Open Access
Clinical Features and Significance of Malignant Priapism
Dilibe C. Ekowa1, Austin J. Marrah2, Justin D. Murray2, Mark R. Wakefield2, 3, Yujiang Fang1,2,3
1Department of Microbiology, Immunology & Pathology, Des Moines University, West Des Moines, IA, 50266, USA.
2Department of Surgery, University of Missouri School of Medicine, Columbia, MO, 65212, USA.
3Ellis Fischel Cancer Center, University of Missouri School of Medicine, Columbia, MO, 65212, USA.
Correspondence: Yuijang Fang (Department of Microbiology, Immunology & Pathology, Des Moines University, West Des Moines, IA, 50266, USA. Email: yuijang.fang@dmu.edu)
Annals of Urologic Oncology 2024, 7(2): 55-60. https://doi.org/10.32948/auo.2024.07.15
Received: 06 Jul 2024 | Accepted: 16 Jul 2024 | Published online: 18 Jul 2024
Priapism is a disorder defined as a persistent erection maintained without an appropriate sexual stimulus lasting for longer than 4 hours. Priapism is generally classified into two categories, ischemic and non-ischemic. Ischemic priapism is considered a true urological emergency as prolongation of this subtype is often associated with loss of sinusoidal endothelial function, corporal fibrosis, and necrosis. Non-ischemic priapism is a type of priapism often caused by the formation of arteriovenous fistulas that create dysregulation of cavernosa blood flow. One less common cause of priapism includes malignancy. Malignancy, either primary or secondary, is considered a rare cause of priapism. During our review of malignant priapism, several etiologies have been identified as potential causes of malignant priapism. Pathologies such as chronic myelogenous leukemia, chronic lymphocytic leukemia, and myelodysplastic syndromes have been implicated in the development of priapism, most likely due to hyperleukocytosis. Metastasis from distal or regional tumors such as the lung, bladder, prostate have been shown to produce secondary tumors that can initiate the development of priapism. Thus, it is important to consider malignancy as a possible cause of a patients priapism. The clinical presentation and prognosis between patients vary greatly and modern treatment modalities have been shown to differ greatly in its efficacy. A comprehensive study that addresses the different forms of malignant priapism may benefit healthcare professionals by providing a better understanding of the complexities, etiologies, and early interventions that can be used for their patients.
Key words Priapism, metastasis, hematologic malignancy, embolization
Malignancy has been thought to be a cause of priapism in some patients. The pathophysiology is mostly unclear but is thought to be a manifestation of mechanical blockage of the corporal cavernosa drainage system. Malignant priapism develops from tumor invasion of the penile compartment. Rarely are cases of malignant priapism caused by primary penile tumors. More often, metastasis or spread from other primary tumors can result in priapism. Cases of hematological cancers, such as chronic lymphocytic leukemia (CLL) and chronic myelogenous leukemia (CML), spread via a hematogenous route and enter the penile compartment resulting in priapism. Regional metastasis may be more likely to induce priapism via direct invasion of tumor mass, as seen in cases of urothelial bladder carcinoma, muscle invasive bladder carcinoma and prostate adenocarcinoma. Distant metastasis of tumor cells such as in the lung, may spread through lymphatic tissue and reach the penis resulting in priapism.
In some cases, priapism may be the initial presenting symptom or complaint [2, 3]. The pathophysiology of malignant priapism is thought to be due to mechanical obstruction. Thus, like other blood dyscrasias like sickle cell, patients present with ischemic priapism [1, 4]. Tissue hypoxia leads to toxic metabolites which cause pain and often times corporal aspiration suggests a hypoxic environment.
Some case studies, however, have demonstrated that malignant priapism can also manifest with non-classical cavernosa blood gas analysis values [5]. In this particular case, the patient presented with signs of ischemic priapism, however aspiration analysis was ambiguous.
Commonly, metastasis is identified as the underlying cause of a patient's priapism. Metastasis depends on the cancer type but generally occurs through hematogenous or lymphatic spread and local invasion. Some studies have demonstrated that metastasis of carcinoma from areas like the lung, rectosigmoid, prostate and bladder have been implicated in the development of priapism in some patients [5, 6, 7]. Spread from distant areas may be explained by lymphatic or hematogenous metastasis of carcinoma. Carcinoma located in regions near the penis, such as bladder and prostate may be better explained by structural invasion as well as metastatic spread. Despite the extensive blood supply of the penis, metastasis to its blood supply is less common than to that of other organ structures. The reason for this is unclear.
Hematological manifestations of malignancy such as chronic myeloid leukemia, chronic lymphocytic leukemia, and myelodysplastic syndromes have been identified as causes of priapism in some patients [2, 8]. It is thought that patients with hematological malignancies associated with priapism may have a more favorable prognosis compared to those with non-hematological factors. The reason for this may be explained by the sensitivities of the primary malignancies to treatment [9]. Nevertheless, failure to address ischemic priapism has been associated with complete loss of erectile function if not addressed within 24 hours [10].
Non-ischemic priapism may develop but it is thought to be less likely. Formation of arteriovenous fistulas from metastatic disease is one implication but data is relatively weak in this area.
Priapism can be due to iatrogenic implications when treating underlying malignancy in patients with priapism. Damage to the penis can precipitate the formation of arteriovenous fistulas and cause a non-ischemic priapism although seldom cases of this has been reported [11]. Figure 1 shows that common characteristics of the two types of priapism.
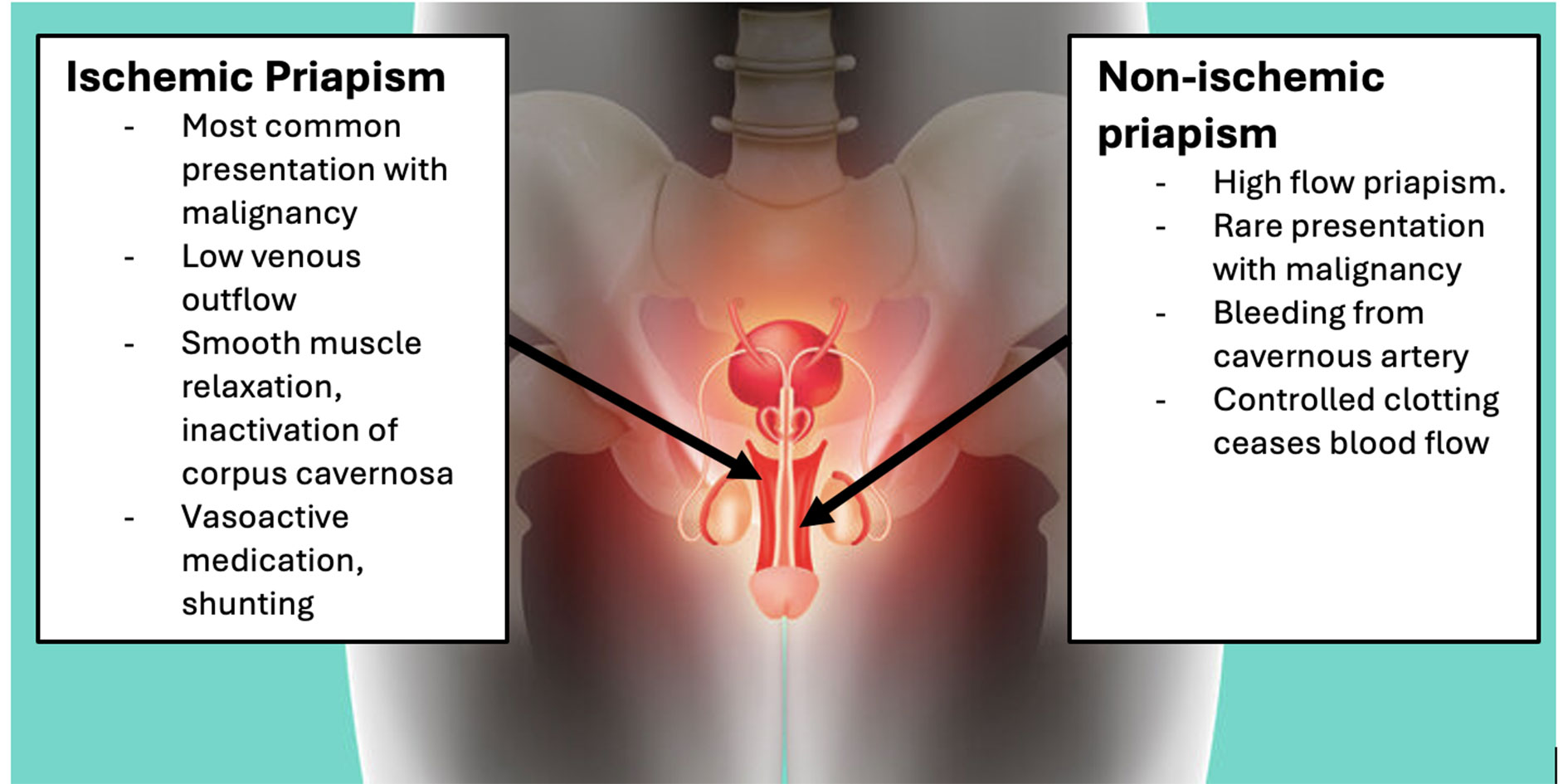 Figure 1. Common characteristics of the two types of priapism. Ischemic priapism (left) and non-ischemic priapism (right) are the two most common types of priapism.
Figure 1. Common characteristics of the two types of priapism. Ischemic priapism (left) and non-ischemic priapism (right) are the two most common types of priapism.
In ischemic priapism, the use of vasoactive drugs is effective because smooth muscle tone is essential in detumescence of priapism. Generally, smooth muscle relaxation is the primary issue causing the maintenance of an erection during priapism. This is opposed to the relatively dilated status of veins seen in the flaccid penis, which allows for proper drainage of the tissue. While there are multitudes of causes for such priapism, including mechanical injury, anticoagulation medications, blood disorders, and various oncological conditions, use of these vasoactive medications are effective in relieving priapism, thereby minimizing its harmful effects [4, 13].
More persistent cases of ischemic priapism generally fall onto shunting between the corpus cavernosum and glans penis so that blood may be released from the penis [11]. This allows for detumescence and aids in restoring normal blood flow throughout the penis [14].
Non-ischemic priapism is generally treated with the use of coagulation to staunch bleeding occurring in the penis. Numerous treatments make use of embolization for cases such as transcatheter embolization and micro-coil embolization to cause controlled clotting within the affected area [15, 16].
Oncology related priapism is unique in its treatment due to the many presentations it has and the mechanisms by which it causes priapism. Tumors may have metastasized to the penis, originated in the penis, or this priapism could be a consequence of hematological malignancy. Regardless of the origin, however, priapism resulting from malignancy presents almost exclusively as ischemic priapism [1].
Patients experiencing drug induced priapism may respond differently to common treatment options if they also suffer from related malignancies. In one such case, a man suffering from muscle invasive bladder cancer experienced priapism from a minimal dose of tadalafil which was taken to treat erectile dysfunction. Despite the low dosage and presentation with common ischemic priapism, treatment with epinephrine was ineffective, requiring a shunt to relieve his condition [6].
Although rare, non-ischemic malignant priapism can result from secondary tumor growth in the penis. One such case is documented, in which a patient presented with a non-painful erection characteristic of non-ischemic priapism. In this case, a biopsy revealed nests of cancer cells that had metastasized to the penis. Recommended treatment for this patient included Sunitinib and radiation therapy, however radiation therapy was refused. In cases like this, however, further cancer treatment should be pursued to limit further metastasis [3].
Priapism in patients suffering from leukemias is a well-documented phenomenon that is believed to be caused primarily by hyperleukocytosis. Treatment for this focuses on addressing the direct cause of the priapism in conjunction with the patient’s underlying condition. This involves the same general treatments for ischemic priapism described earlier, largely by using vasoactive and surgical options in addition to the patient’s oncologic treatments [17, 18, 19].
It should be noted that it is commonplace to expand oncologic treatments in response to the presentation of malignant priapism. Doing so using cancer targeting drugs such as kinase inhibitors sunitinib or imatinib has seen varying success in treating metastatic priapism resulting from kidney cancer and leukemia [2, 3].
As priapism is related to secondary penile metastasis, such as bladder and prostate cancer, this can be a sign of a more serious case of malignant cancer as the average life expectancy of patients with malignant priapism averages around 9 months with a maximum of 18 months usually being the longest recorded survival [5, 20, 21, 22, 23, 24, 25, 26, 27].
In a systematic review of penile metastasis and malignant priapism, Andrea Cocci and her group were able to identify 69 cases of penile metastasis from 2003 to 2013, with metastases being located on the root (38.8%), the shaft (38.8%) and the glans (22.2%) of the penis. Of these cases, ten patients have been reported to have priapism. In their review, they performed a Kaplan-Meier curve analysis comparing patients with metastasis, finding that cases with malignant priapism had a worse prognosis than those without priapism [26].
This data is consistent with a literature review that analyzed 29 cases of penile metastasis – 7 cases presenting priapism – and found that the prognosis of secondary penile malignancies averaged approximately 9 months, with an overall survival of less than 18 months [20].
It should be noted that life expectancy should be determined based on the etiology of cancer [22, 24, 28]. One study shows that patients with rectal primary tumors who developed malignant priapism have the longest survival time being 7 and 9 years with a median survival of 18 months since the last surgical treatment [20, 21, 27]. Additionally, Andrea Cocci and her group were able to identify 10 patients who presented with priapism as the first symptom – 5 from urological and 5 from non-urological cancers – and determined that patients with urological cancer had a greater median survival time of 30 months compared to patients with non-urological cancers at 15 months [26].
However, despite these outliers and how penile metastasis spreads, prognoses of secondary penile malignancies – including malignant priapism – remain poor, with the majority of patients surviving less than 18 months regardless of treatment. Table 1 shows that cases of priapism, treatment and outcomes.
|
Table 1. Cases of priapism, treatment and outcomes. |
|||||
|
Study referenced |
Priapism duration |
Ischemic/non-ischemic |
Primary tumor |
Treatment |
Resolution |
|
[2] |
6d |
I |
Bone marrow |
1.) Imatinib, shunting |
1.) R |
|
[3] |
10d |
N |
Kidney |
1.) Sunitinib |
1.) PI |
|
[5] |
15d |
I |
Tcell |
1.) Norepinephrine, percutaneous aspiration 2.) Shunting |
1.) PI 2.) TI |
|
[5] |
1d |
I |
Bone marrow |
1.) Corporal wash 2.) Shunting 3.) Cavernotomy |
1.) TI 2.) TI 3.) R |
|
[6] |
3d |
I |
Bladder |
1.) Norepinephrine 2.) Shunting |
1.) NE 2.) NR |
|
[17] |
56d |
I |
Prostate |
1.) Radiotherapy, pudenal nerve block, hormonal therapy |
1.) NR |
|
[19] |
20d |
I |
Bone marrow |
1.) Leukapheresis 2.) intracavernous aspiration 3.) Leukapheresis imatinib, |
1.) TI 2.) TI 3.) R |
|
[20] |
90d |
I |
Prostate |
1.) Cavernostomy |
1.) NE |
|
[22] |
14d |
I |
Bladder |
1.) Analgesia pump 2.) Penectomy |
1.) TI 2.) R |
|
[22] |
Several d |
I |
bladder |
1.) Distal shunting 2.) Penectomy |
1.) NR 2.) R |
|
[22] |
Several d |
I |
Prostate |
1.) Penile ring block 2.) Penectomy |
1.) TI 2.) R |
|
[29] |
NR |
I |
Prostate |
1.) Pelvic radiotherapy |
1.) R |
|
[30] |
60d |
NR |
Testicle |
1.) Intracorporeal aramine 2.) orchiectomy |
1.) NE 2.) NE |
|
[31] |
30d |
I |
Skin |
1.) Shunting 2.) Surgical tumor removal |
1.) NE 2.) NR |
|
Key: Days of priapism - #d, Hours of priapism - #h, Ischemic priapism - I, Non-ischemic priapism - N, Priapism resolved - R, Priapism improved - PI, Temporary improvement - TI, No effect - NE, Not reported - NR. |
|||||
None.
Ethical policy
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Approval from institutional ethical committee was taken.
Availability of data and materials
All data generated or analysed during this study are included in this publication.
Author contributions
Yujiang Fang initiated the idea and supervised the whole process. Dilibe C. Ekowa, Austin J. Marrah, and Justin D. Murray wrote the draft. Mark R. Wakefield and Yujiang Fang made critical revisions to the draft.
Competing interests
Authors report no conflict of interest.
Funding
This study was partially supported by the grant for Yujiang Fang (IOER 112-3119).
- Marcu D, Iorga L, Mischianu D, Bacalbasa N, Balescu I, & Bratu O: Malignant Priapism - What Do We Know About It? In vivo (Athens, Greece) 2020, 34(5): 2225-2232.
- Shaeer OK, Shaeer KZ, AbdelRahman IF, El-Haddad MS, & Selim OM: Priapism as a result of chronic myeloid leukemia: case report, pathology, and review of the literature. J Sex Med 2015, 12(3): 827-834.
- Luo Y, Yang F, Cai J, Li W, & Zhan H: Malignant priapism as the initial presentation induced by the metastasis of renal clear cell carcinoma after radical nephrectomy. Urol Case Rep 2021, 39: 101795.
- Yuan J, Desouza R, Westney OL, & Wang R: Insights of priapism mechanism and rationale treatment for recurrent priapism. Asian J Androl 2008, 10(1): 88-101.
- Prabhuswamy VK, Krishnappa P, & Tyagaraj K: Malignant refractory priapism: An urologist's nightmare. Urol Ann 2019, 11(2): 222-225.
- Prabharani D, & Pramod SV: Single dose Tadalafil 5 mg in Muscle Invasive Bladder Cancer (MIBC) patient induce priapism: A case report and literature review. Urol Case Rep 2022, 45: 102200.
- De Luca F, Zacharakis E, Shabbir M, Maurizi A, Manzi E, Zanghì A, De Dominicis C, & Ralph D: Malignant priapism due to penile metastases: Case series and literature review. Arch Ital Urol Androl 2016, 88(2): 150-152.
- James Johnson M, Hallerstrom M, Alnajjar HM, Frederick Johnson T, Skrodzka M, Chiriaco G, Muneer A, & Ralph DJ: Which patients with ischaemic priapism require further investigation for malignancy? Int J Impot Res 2020, 32(2): 195-200.
- Marcu D, Iorga L, Mischianu D, Bacalbasa N, Balescu I, & Bratu O: Malignant Priapism - What Do We Know About It? In vivo (Athens, Greece) 2020, 34(5): 2225-2232.
- Pryor J, Akkus E, Alter G, Jordan G, Lebret T, Levine L, Mulhall J, Perovic S, Ralph D, & Stackl W: Priapism. J Sex Med 2004, 1(1): 116-120.
- Silberman, Ml: Priapism. StatPearls [Internet]. 2023.
- Vorobets D, Banyra O, Stroy A, & Shulyak A: Our experience in the treatment of priapism. Cent European J Urol 2011, 64(2): 80-83.
- Broderick GA, Gordon D, Hypolite J, & Levin RM: Anoxia and corporal smooth muscle dysfunction: a model for ischemic priapism. J Urol 1994, 151(1): 259-262.
- Cherian J, Rao AR, Thwaini A, Shergill IS, & Samman R: Medical and surgical management of priapism. Oxford Academic 2006.
- Numan F, Cantasdemir M, Ozbayrak M, Sanli O, Kadioglu A, Hasanefendioglu A, & Bas A: Posttraumatic Nonischemic Priapism Treated with Autologous Blood Clot Embolization 2008. Science Direct.
- Abujudeh H, Mirsky D: Traumatic high-flow priapism: treatment with super-selective micro-coil embolization. Emerg Radiol 2005, 11: 372-374.
- Bintoro SUY, Romadhon PZ, Suryantoro SD, Aminy RZ, Windradi C, & Widiyastuti KN: Case Report: Priapism as The Clinical Presenting Feature of Chronic Myeloid Leukemia: Case Report and 20-Year Literature Review. F1000 Research 2022, 10: 571.
- Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JPW, Lue TF, Nehra A, & Sharlip ID: American Urological Association Guideline On The Management of Priapism. AUA Journals 2003, 170(4 Pt 1): 1318-1324.
- Gaye O, Thiam NM, Cassell A, Gueye SM, Sow Y, Fall B, & Ndoye AK: Unusual Presentation of Priapism Associated with Acute and Chronic Myeloid Leukemia in Two Patients: Emergency Management. Case Rep Urol 2020, 2020: 4982432.
- Lin Y-H, Kim JJ, Stein NB, & Khera M: Malignant priapism secondary to metastatic prostate cancer: A case report and review of literature. Rev Urol 2011, 13(2): 90-94.
- Sibarani J, Syahreza A, Wijayanti Z, Atik TN, & Rachmadi D: Malignant priapismus induced by adenocarcinoma of the prostate. Urol Case Rep 2020, 29: 101102.
- Tabei SS, Baas W, Brooks A, Kim EH, Smith Z, & Murphy GP: Malignant priapism: case report and update on management protocols. Transl Androl Urol 2023, 12(10): 1607-1613.
- Ralph O, Shroff N, Johnson MJ, AlNajjar HM, & Ralph D: Malignancy: A Rare, Important and Poorly Understood Cause of Priapism. Sex Med Rev 2021, 9(2): 312-319.
- Yudiana IW, Sugianto R, Putri PED, Ekawati NP, & Duarsa GWK: The Current Challenges in Diagnosing and Treating Malignant Priapism: A Comprehensive Review. Urol Res & Pract 2023, 49(6): 360-364.
- Spinapolice EG, Fuccio C, Rubino B, Palumbo R, Mensi M, Scopesi L, Trifirò G, & Ivaldi GB: Penile metastases from bladder and prostate cancer detected by PET/CT: a report of 3 cases and a review of literature. Clin Genit Cancer 2014, 12(4): e155-e159.
- Cocci A, Hakenberg OW, Cai T, Nesi G, Livi L, Detti B, Minervini A, Morelli G, Carini M, Serni S, & Gacci M: Prognosis of men with penile metastasis and malignant priapism: a systematic review. Oncotarget 2017, 9(2): 2923-2930.
- Chaux A, Amin M, Cubilla AL, & Young RH: Metastatic tumors to the penis: a report of 17 cases and review of the literature. Int J Surg Pathol 2011, 19(5): 597-606.
- Cherian J, Rajan S, Thwaini A, Elmasry Y, Shah T, & Puri R: Secondary penile tumours revisited. Int Semi Surg Oncol 2006, ISSO, 3: 33.
- Xing DT, Yilmaz H, Hettige S, Hegde R, & Nair R: Successful Treatment of Malignant Priapism by Radiotherapy: Report of a Case, Review of the Literature, and Treatment Recommendations. Cureus 2021, 13(8): e17287.
- Jiang J, Zhu X, SHI S, Xie L, Teng X, Chen Z, & Zheng X: Malignant priapism secondary to testicular tumor. Chin Med J (Engl) 2009, 122(15): 1839-1840.
- Okinami T, Ishitoya S, Imamura M, Maeda S, Okumura K, & Nose K: A case of penile metastasis of malignant melanoma with priapism. Hinyokika Kiyo 2009, 55(3): 149-152.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript