Case Report | Open Access
Urinary Bladder Leiomyoma Causing Obstructive Uropathy: A Case Report and Literature Review
Karthikesh Omkaram1, Ramprasad Reddy A1, Ershad Hussain Galeti2, Surender Reddy1, Mohammed Abdul Aleem3, Gousia Begum S4
1Department of Urology, Sri Srinivasa Kidney Centre, Hanamkonda, Telangana, India.
2Department of General Surgery and Urology, Viswabharathi Medical College, Kurnool, Andhra Pradesh, India.
3Department of Pathology, Unipath Speciality Laboratory Limited, Hyderabad, India.
4Department of Anaesthesia, Viswabharathi Medical College, Kurnool, Andhra Pradesh, India.
Correspondence: Ershad Hussain Galeti (Department Of General Surgery and Urology, Viswabharathi Medical College, Kurnool, 518463, Andhra Pradesh, India; Email: dr.ershadhussain@gmail.com).
Annals of Urologic Oncology 2023, 6(1): 27- 31. https://doi.org/10.32948/auo.2023.01.24
Received: 02 Jan 2023 | Accepted: 24 Jan 2023 | Published online: 27 Jan 2023
Key words leiomyoma, benign tumour, urinary bladder neoplasm, open excision
Ultrasound examination of the abdomen revealed a 5 × 5 cm smooth lesion (Figure 1) with peripheral hyperechogenicity arising from the base of the bladder near left vesicoureteral junction (VUJ) and a left moderate hydroureteronephrosis and also right small kidney with mild hydronephrosis. Non-contrast computerized tomography of kidney, ureter and bladder revealed a well-defined heterogeneous hypodense mass lesion measuring 57 × 54 mm in the lumen of urinary bladder arising from the base of bladder at the site of left VUJ with moderate hydroureteronephrosis and right contracted kidney with mild hydronephrosis (Figure 2).
On cystoscopy, a 6 × 5 cm endovesical tumour arising from the base of the bladder near the left VUJ was seen. Bilateral double J ureteric stents were inserted due to obstructive uropathy. After 2 weeks, serum creatinine was reduced to 79.5?mol/L and blood urea was 7.5mmol/L.
Transurethral resection of the bladder tumor was performed with a few biopsies taken for histopathological examination. The surgery was uncomplicated. Histopathology showed intersecting fascicles of spindle cells with an elongated nucleus that were separated by connective tissues with the occasional focus of necrosis with no mitotic activity and no cellular atypia (Figure 3). On immunohistochemistry, cells had positive staining for smooth muscle actin, H. caldesmon and negative staining for Ki-67 suggesting leiomyoma of the urinary bladder.
Surgical exploration was undertaken via a lower midline incision. Urinary bladder is approached extraperitoneally, mobilised and anterior wall was incised. An endovesical bladder tumor of size 6 x 5 cm was found at the base near left VUJ with normal mucosa over the tumor (Figure 4). As it was a benign tumor on histopathology, mucosa was incised and a good plane of cleavage was found between the tumor and bladder wall. Tumor was excised completely after ligating its pedicle and was sent for histopathology. Grossly, it was white-gray in color and the surface was nodular (Figure 5). Pathological diagnosis of excised tumor was leiomyoma. The patient's recovery was uncomplicated, and patient was discharged one week later. During the follow-up for 24 months, the patient remained asymptomatic without any lower urinary tract symptoms.
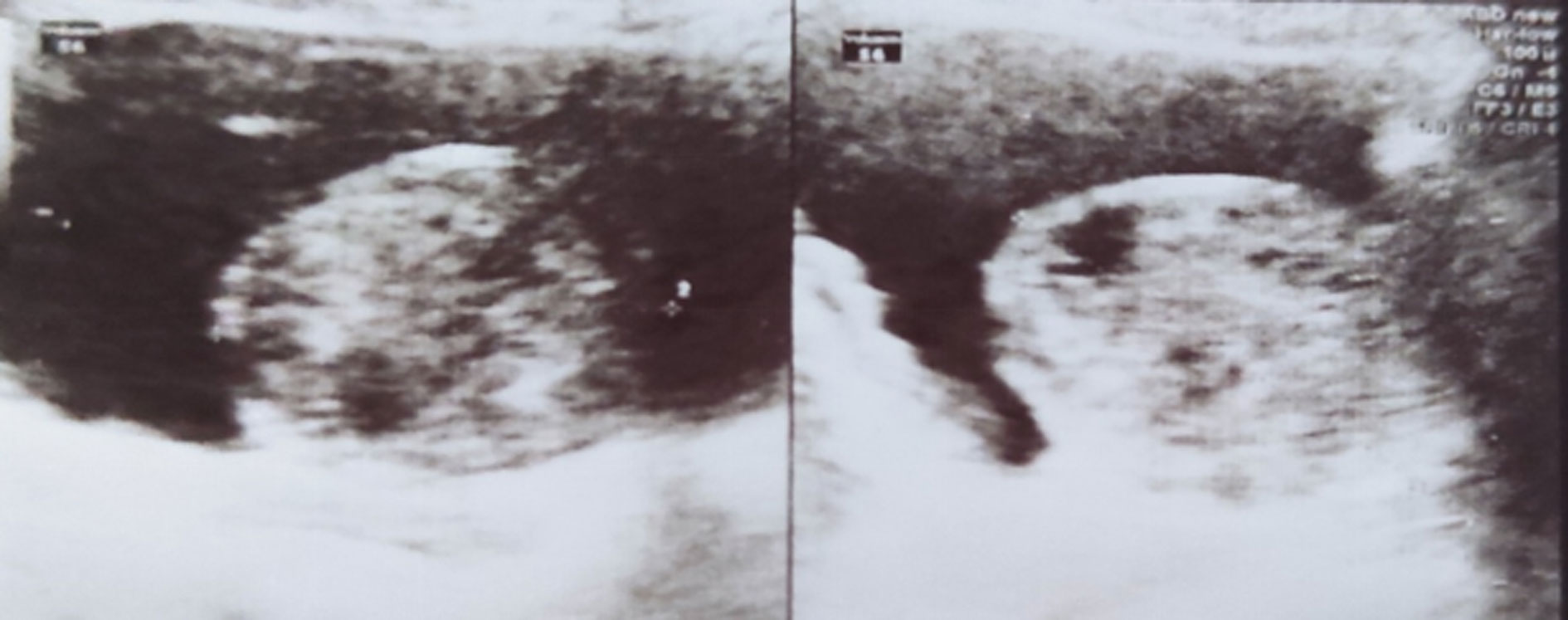 Figure 1. Ultrasound Abdomen showing showing a smooth endovesical bladder lesion with peripheral hyperechogenicity.
Figure 1. Ultrasound Abdomen showing showing a smooth endovesical bladder lesion with peripheral hyperechogenicity.
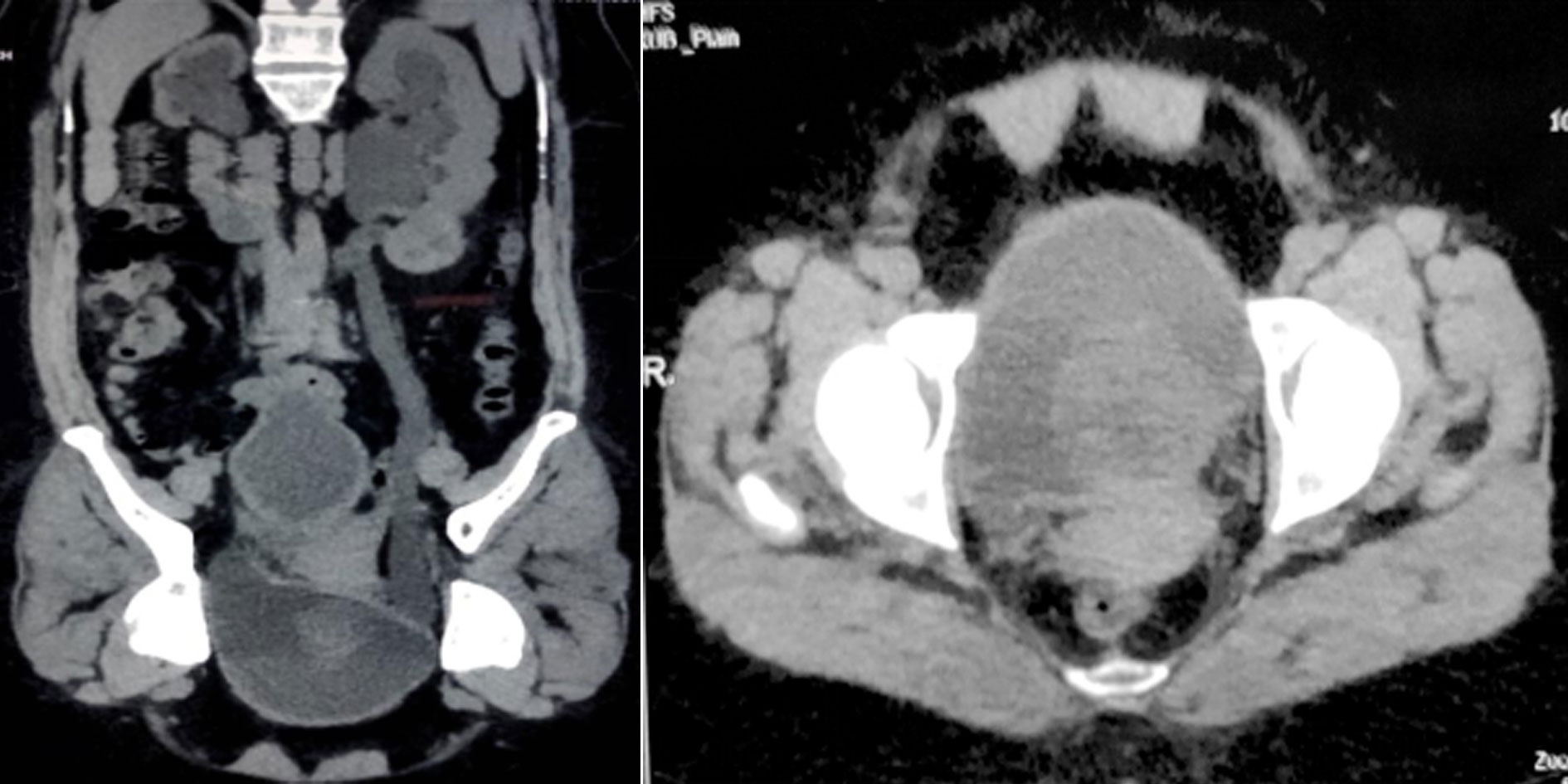 Figure 2. Non-contrast Computerized Tomography of KUB showing a well-defined heterogeneous hypodense mass lesion of size approximately 57 × 54 mm noted in the lumen of urinary bladder arising from the base of bladder at the site of left VUJ with moderate hydroureteronephrosis and right contracted kidney with mild hydronephrosis.
Figure 2. Non-contrast Computerized Tomography of KUB showing a well-defined heterogeneous hypodense mass lesion of size approximately 57 × 54 mm noted in the lumen of urinary bladder arising from the base of bladder at the site of left VUJ with moderate hydroureteronephrosis and right contracted kidney with mild hydronephrosis.
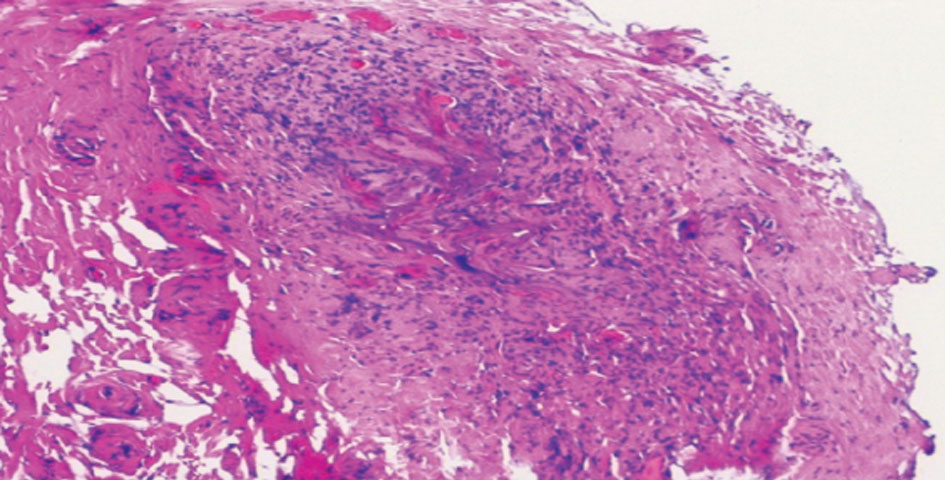 Figure 3. TURBT chips for histopathology showed proliferation of spindle-shaped cells and eosinophilic cytoplasm with no atypical mitotic figures (H and E, 100x).
Figure 3. TURBT chips for histopathology showed proliferation of spindle-shaped cells and eosinophilic cytoplasm with no atypical mitotic figures (H and E, 100x).
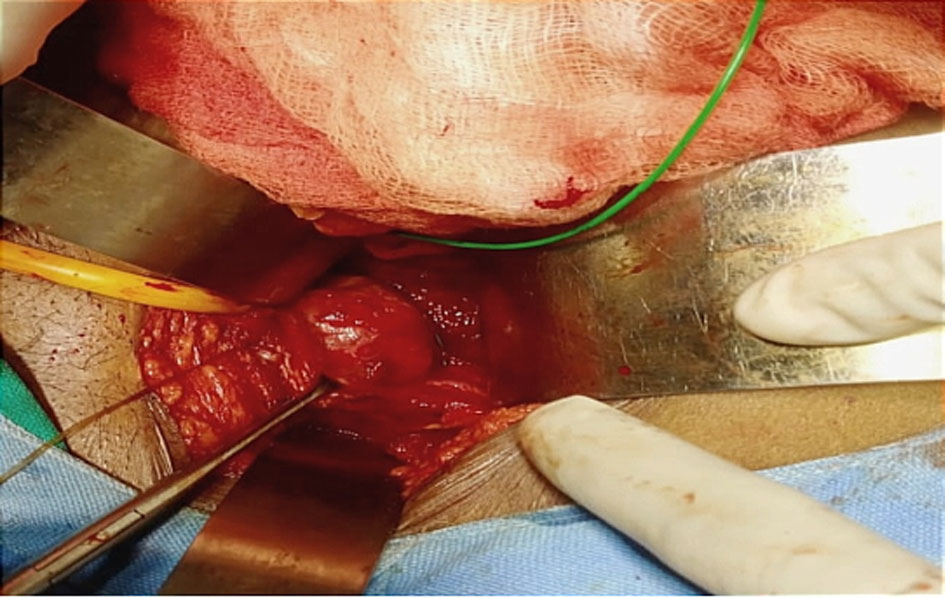 Figure 4. Intraoperative picture showing bladder leiomyoma after anterior cystostomy.
Figure 4. Intraoperative picture showing bladder leiomyoma after anterior cystostomy.
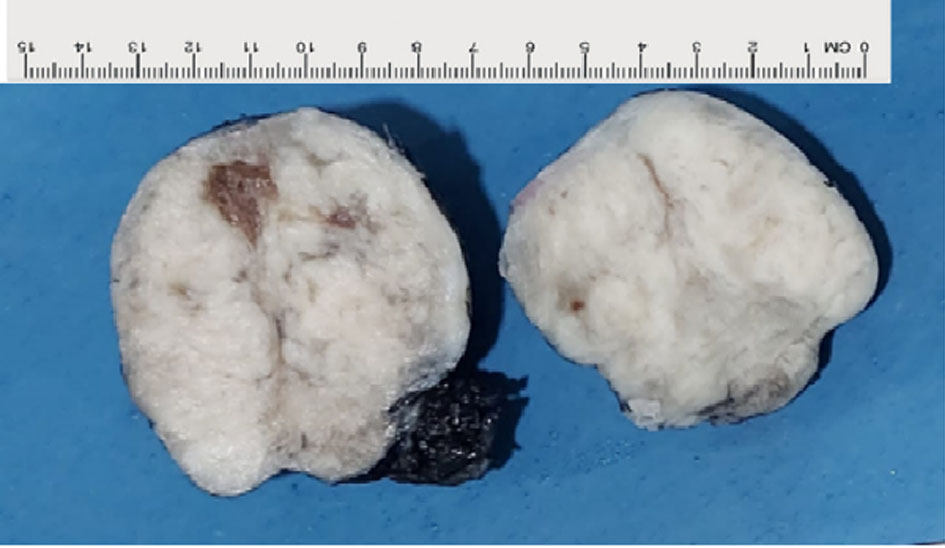 Figure 5. Gross pathology of the tumor showing well circumscribed bulging mass with rubbery in consistency which was white-gray in color and had a nodular surface.
Figure 5. Gross pathology of the tumor showing well circumscribed bulging mass with rubbery in consistency which was white-gray in color and had a nodular surface.
These tumours can be endovesical, intramural, or extravesical. Endovesical tumours are the most frequent and often present with dysuria, urine urgency, hematuria, and, in rare cases, low back pain. Some tumours are pedunculated and can cause urine retention [11, 12].
In regards to diagnosis, bladder ultrasonography is the imagiologic examination that detects these tumours the most often. In most cases, it appears as a tiny solid mass that is uniform and hypoechoic, encompassed by a narrow hyperechogenic blade [7]. Cystoscopy reveals the presence of a sessile tumour that is not arborescent and protrudes into the bladder lumen. Computed tomography and magnetic resonance imaging (MRI) can be used to determine the size and location [13]. For the composition and relation to plains of the bladder wall, MRI is the ideal approach. Regardless of the imaging characteristics, histopathology is the definitive diagnosis [11].
In the series of Kabalin et al. [14] and Chavez and Neto [15], among the 35 patients who had the bladder leiomyoma excised, only two had residual tumour and needed a re-excision. This low re-intervention rate means that regardless of the excisional method, bladder leiomyoma is adequately and easily treated, with almost no recurrence when fully resected. The exact location, size, extent and potential involvement of the ureters or sphincter will determine which of these therapies is the most appropriate. As a general rule, small endovesical bladder leiomyomas can be treated by TURBT, but larger intramural or extravesical ones are treated by open resection. It is mandatory to make sure that the ureteric orifice will not be obstructed by any residual tumour that initially caused potential hydronephrosis. Some surgeons would advocate taking a retrograde pyelogram and inserting a ureteric stent to avoid the postoperative local oedema causing a persistent pelvicalyceal dilatation.
Leiomyomas of the urinary bladder share common histopathological features with leiomyomas of the uterus, i.e. round nodules, grey-white, with a spiral appearance of smooth muscle fibres gathered in small fascicles and separated by varying amounts of fibrous connective tissue, and fewer than two mitotic figures per high-power field [6].
The endovesical subtype is more common because it bulges into the bladder, resulting in more symptoms and causing the patient to seek medical attention. As the endovesical site is the most common location, corresponding to 63–86% of the cases, TURBT represents the main treatment in almost 90% of cases, unless a large intramural leiomyoma is encountered (3–7%) or an extravesical one (11-30%) [6,10], requiring a wider excision, like a partial cystectomy. Treatment and prognosis is determined primarily according to the size and anatomical location of the tumors. Surgical excision has an excellent prognosis and should always be offered. Moreover, transurethral resection is a safe and effective initial choice for patients with relatively smaller tumors. Larger tumors and those with extravesical growth usually require open surgery with segmental resection or partial cystectomy [17].
The pathophysiology of these lesions remains unknown but four theories have been proposed: (1) Hormonal disturbances cause these tumours to develop; (2) Dysontogenesis, e.g. embryonic rests of tissue residing in the bladder that transform into leiomyomas; (3) Perivascular inflammation leading to metaplastic transformation of the bladder vascular supply; and (4) Bladder musculature infection leading to inflammation and the development of these benign tumours [16]. More studies and research are needed to elucidate the mechanism of their growth.
Surgical treatment, when the excision is wide enough, is almost always very effective, leaving a very low recurrence rate, and with no symptoms, confirming the benign nature of bladder leiomyomas and their excellent prognosis.
We extend our sincere thanks to the patient who participated in the study.
Ethical policy
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Approval from institutional ethical committee was taken.
Informed consent
Informed consent was obtained from the participant included in the study. Approval from institutional ethical committee was taken.
Availability of data and materials
All data generated or analysed during this study are included in this publication.
Author contributions
Conception and design of study: Dr. Ramprasad Reddy A, Dr. Surender Reddy; Acquisition of data: Dr. Karthikesh Omkaram, Dr. Ershad Hussain Galeti, Dr. Mohammed Abdul Aleem; Analysis and/or interpretation of data: Dr. Karthikesh Omkaram, Dr. Ershad Hussain Galeti, Dr. Gousia Begum S; Drafting the manuscript: Dr. Ershad Hussain Galeti, Dr. Karthikesh Omkaram, Dr. Mohammed Abdul Aleem; Revising the manuscript critically for important intellectual content: Dr. Karthikesh Omkaram, Dr. Ershad Hussain Galeti, Dr. Gousia Begum S; All authors read and approved the final manuscript.
Competing interests
No conflict of interest.
Funding
None.
- Cornella JL, Larson TR, Lee RA, Magrina JF, Kammerer-Doak D: Leiomyoma of the female urethra and bladder: report of twenty-three patients and review of the literature. Am J Obstet Gynecol 1997, 176(6): 1278-1285.
- Saunders SE, Conjeski JM, Zaslau S, Williams J: Leiomyoma of the urinary bladder presenting as urinary retention in the female. Can J Urol 2009, 16(4): 4762-4764.
- Campbell EW, Gislason GJ: Benign mesothelial tumors of the urinary bladder: a review of the literature and a report of ease of leiomyoma. J Urol 1953, 70(5): 733-742.
- Melicow MM: Tumours of the urinary bladder. J Urol 1937, 37: 117.
- De Berne-Lagarde A: Les leiomyomes vesicaux. Arch D Mal des Reins Des Organes Genitourin 1929, 4: 412-441.
- Knoll LD, Segura JW, Scheilhauer BW: Leiomyoma of the bladder. J Urol 1986, 136(4): 906-913.
- Khater N, Sakr G: Bladder leiomyoma: Presentation, evaluation and treatment. Arab J Urol 2013, 11(1): 54-61.
- Mutchler RW, Gorder JL: Leiomyoma of the bladder in a child. Br J Radiol 1972, 45(535): 538-540.
- Kutzmann AA: Leiomyoma of urinary bladder. J Urol 1937, 37: 117-132.
- Goluboff ET, O’Toole K, Sawczuk IS: Leiomyoma of bladder: report of case and review of literature. Urology 1994, 43(2): 238-241.
- Pardal H, Ferronha F, Gameiro C, Vilas-Boas V, Galego P, Melo P: Intramural vesical leiomyoma in a patient with a pelvic fibrous tumour - case report. Acta Urol 2011, 2: 28-31.
- Kim IY, Sadeghi F, Slawin KM: Dyspareunia: An unusual presentation of leiomyoma of the bladder. Rev Urol 2001, 3(3): 152-154.
- Silva-Gutiérrez A, Martínez-Méndez ME, González-Romo MA, Nava-Jácome O, Castillo-Zurita O, Morales-Díaz J: Bladder leiomyoma. Rev Mex Urol 2013, 73: 43-45.
- Kabalin JN, Freiha FS, Niebel JD: Leiomyoma of bladder: report of 2 cases and demonstration of ultrasonic appearance. Urology 1990, 35(3): 210-212.
- Chavez CA, Neto M: Multiple leiomyomata of the urinary bladder. J Kans Med Soc 1984, 85(11): 298-299.
- Teran AZ, Gambrell RD: Leiomyoma of the bladder. Int J Fertil 1989, 34(4): 289-292.
- Itam S, Elhage O, Khan MS: Large leiomyoma of the bladder masquerading as an enlarged prostate gland. BMJ Case Rep 2016, 2016: bcr2015212800.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript