Research Article | Open Access
Correlation between Serum PSA, Gleason Score and Histopathological Grading of Adenocarcinoma of Prostate in Patients Undergoing TRUS Guided Prostatic Biopsy in a Tertiary Care Centre of Southern India
Veda Murthy Reddy Pogula1, Karthikesh Omkaram1, Ershad Hussain Galeti1, Bhargava Reddy Kanchi V1
1Narayana medical college, Nellore, Andhra Pradesh, India.
Correspondence: Ershad Hussain Galeti (Narayana medical college, Nellore, Andhra Pradesh, India; Email: dr.ershadhussain@gmail.com).
Annals of Urologic Oncology 2021, 4(1): 42-47. https://doi.org/10.32948/auo.2021.12.06
Received: 15 May 2021 | Accepted: 06 Dec 2021 | Published online: 20 Dec 2021
Background Prostate cancer is the second most common cancer and the fifth leading cause of cancer deaths worldwide. Serum psa, a glycoprotein and a serine protease, which is increased in all prostatic diseases but markedly elevated levels are indicative of carcinoma prostate. The present study was done to evaluate the histopathologyof carcinoma of prostate in trus guided prostatic biopsy specimens and correlate serum psa levels with gleason score and grade groups.
Methods A hundred patients presented with luts and suspicious of carcinoma prostate underwent trus guided 16 core prostatic biopsy. Histopathological examination, gleason scores and grades of biopsies were obtained. Based on the gleason scores, patients with carcinoma of the prostate were divided into five-grade groups. Mean serum psa levels were calculated and correlated with gleason score and grade groups.
Results Malignancy was found in 69 per cent of cases, of which 68 patients were found to have adenocarcinoma of the prostate, one patient found to have undifferentiated carcinoma of the prostate. The total number of patients in each gleason grade groups were obtained, and the mean serum psa levels of these patients in each group were calculated. Mean serum psa levels in each group are group 1 (21.3 ng/ml), group 2 (58.4 ng/ml), group 3 (73.6 ng/ml), group 4 (118.4 ng/ml), group 5 (96.3 ng/ml).
Conclusion Serum psa is a highly sensitive tumour marker with low specificity, and its levels are increased in many benign and iatrogenic conditions. Psa has a high negative predictive value which is essential in ruling out malignancy. In our study, higher serum psa levels were correlated with higher gleason score and grades.
Key words Serum PSA, gleason score and grade, carcinoma prostate, lower urinary tract symptoms (LUTS)
Initially developed as a biomarker for monitoring prostate cancer patients after treatment, PSA continues to be a lightning rod for controversy in the setting of prostate cancer screening. Given its unique prominence, a clear understanding of PSA is needed to lay the foundation for other potential prostate cancer biomarkers. Also known as hK3 (human kallikrein 3), PSA is a member of the kallikrein gene family [5]. This is a serine protease, and genes for PSA is located on the long arm of chromosome 19 within the region spanning q13.2-q13.4. Serum PSA, a glycoprotein and a serine protease identified by Wang et al. (1979), is produced exclusively by the epithelial cells of benign and malignant prostatic tissue with normal levels of 0-4ng/ml [6]. PSA levels are increasingly seen in all prostatic diseases, but markedly elevated levels indicate carcinoma prostate.
Histological type, grading & staging of prostate carcinoma is crucial in planning treatment strategies & predicting overall and cancer-specific survival. Various histological grading systems have been developed to correlate with the prognosis of the disease.
The Gleason system is based on the glandular pattern of the tumour as identified at relatively low magnification [7]. Cytologic features play no role in the grade of the tumour. Gleason grading is one of the most best predictors of biological behaviour and influential factors used to determine prostate carcinoma treatment. PSA, when combined with the Gleason score and clinical staging, improves the forecast of pathological staging for prostate Carcinoma. Architectural designs are identified and allocated a grade from 1 to 5, with most differentiated is grade 1 and undifferentiated is grade 5. Although in the original Gleason system, the most common and second most common grades were combined, in 2005, the Gleason system was updated and modified with one change being that on biopsy, the most common and highest-grade patterns on a given core were added to result in the Gleason score [8]. In theory, however, the Gleason scores range from 2 (1 + 1 = 2) to 10 (5 + 5 = 10), representing uniformly composed tumours of Gleason pattern 1 tumour in score 2 to undifferentiated tumours in score 10. It is not recommended that Gleason score 2 to 4 be assigned for adenocarcinoma of the prostate on needle biopsy because assigning a Gleason score of 2 to 4 to an adenocarcinoma on needle biopsy is not necessarily associated with such favourable findings at radical prostatectomy [9]. Gleason score of less than 6 are commonly low-grade cancers and are not aggressive. Gleason score of 8 and above are usually advanced tumours with locoregional spread and distant metastasis. Digital rectal examination, transrectal ultrasonography and serum prostate-specific antigen represent a diagnostic triad to detect prostatic carcinoma. The present study was done to evaluate the histopathology of carcinoma of prostate in TRUS guided prostatic biopsy specimens and correlate serum PSA levels with Gleason score and grade groups.
The aim of this study is to correlate between Serum PSA, Gleason Score and histopathological grading of adenocarcinoma of prostate in patients undergoing TRUS guided prostatic biopsy.
This is a single institutional prospective observational study conducted in the Department of Urology. The duration of the study was two years, from January 2019 to December 2020. The study was done after obtaining patient consent and approval from institutional ethical committee. This study included 100 patients who presented with lower urinary tract symptoms (LUTS). 100 patients who presented with LUTS and suspicious of carcinoma prostate underwent TRUS guided 16 core prostatic biopsy and serum PSA estimation. The PSA levels were estimated in the Biochemistry department. The PSA levels were measured using the CIBA-CORNING automated chemiluminescence system which measures PSA by sandwich assay. All the biopsy specimens underwent proper histopathological examination with Paraffin-embedded hematoxylin, and eosin stain sections and Gleason scores were derived. Cut-off point for abnormal serum PSA was taken as a value of above 4 ng/ml.
Based on the Gleason scores, patients with carcinoma of the prostate were classified into five grade groups, Group 1(score of 3+3=6), Group 2 (score of 3+4=7), Group 3 (score of 4+3=7), Group 4 (score of 4+4=8), Group 5 (score of 9-10). Mean serum PSA levels of patients in each group were calculated and correlated with Gleason score and grading.
Our study was conducted on 100 patients presented with LUTS over two years. The majority [90%] of the patients presented with frequency, Nocturia and postvoid dribbling. Six patients presented with hematuria, and 4 patients with acute urinary retention.
Out of 100 patients, 79 patients were having abnormal serum PSA levels and underwent TRUS guided 16 core prostatic biopsy. Out of these 79 patients, 65 patients were found to have adenocarcinoma of the prostate, one patient found to have undifferentiated carcinoma of the prostate, 10 patients were found to have Benign Prostatic Hyperplasia, and 3 patients were found to have chronic prostatitis.
Twenty-one patients underwent 16 core prostatic biopsy because of abnormal DRE and TRUS findings despite normal serum PSA. Out of 21 patients, 3 patients were found to have adenocarcinoma, 16 had Benign Prostatic Hyperplasia, and 2 had chronic prostatitis.
The majority of cancer patients in this study were in the 7th and 8th decade with a mean age of 71 years. The youngest patient was 47 yrs of age.
Out of 69 patients with carcinoma of the prostate, 24 were found to have a perineural invasion, and a majority of these patients belong to Gleason grade group 4 and 5.
All the cases of prostatic adenocarcinoma were categorized according to Gleason's grading system. A primary and a secondary grade were given, and by adding the both grades, Gleason's score was given. As all 100 patients underwent TRUS guided 16 core prostatic biopsy, the Gleason’s score in the present study ranged from 6 to 10. S.PSA level is correlated with the Gleason score and grade. The increased serum PSA in prostate malignancy cases was evaluated, taking histopathology as the standard test. The results were elucidated as follows: True positive (TP) are cases with high level of serum PSA correctly interpreting malignancy (n=66). True negative (TN) are cases with normal levels of serum PSA correctly ruling out malignancy (n=18). False-positive (FP) are cases with increased level of serum PSA wrongly interpreting nonmalignant cases (n=13). False-negative (FN) are cases with normal level of serum PSA wrongly interpreting malignant cases (n=3). The sensitivity of the serum PSA test in our study is 95.6%. It is a likelihood that the patient with the disease has positive test results. The specificity of the PSA test in our study is 58.0% which suggests that the probability that the patients without disease has negative test results. The positive predictive value is 83.5 which suggests that the probability that patients with a positive screening test truly have the disease. The negative predictive value is 85.7% which suggests that the probability that subjects with a negative screening test genuinely don't have the disease (Table 1).
Fifteen patients were found to have a Gleason score of 3+3 with a mean serum PSA of 21.3 ng/ml (Figure 1). Twenty-one patients were found to have a Gleason score of 3+4 with a mean serum PSA of 58.4 ng/ml. Eighteen patients were found to have a Gleason score of 4+3 with a mean serum PSA of 73.6 ng/ml (Figure 2). Nine patients were found to have a Gleason score of 4+4 with a mean serum PSA of 118.4 ng/ml. Six patients were found to have Gleason score 4+5; 5+4; 5+5 with a mean serum PSA of 96.3ng/ml. One patient had undifferentiated carcinoma of the prostate with a Gleason score of 5+5 and had a serum PSA of 7.02 ng/ml. Three patients with adenocarcinoma of the prostate have normal serum PSA with Gleason score 3+4 and 4+3. Eight patients had serum PSA within 4–10 ng/ml range, and five patients who had serum PSA within 10–20 ng/ml range showed benign prostatic hyperplasia and chronic prostatitis on biopsy (Table 2, 3 and 4).
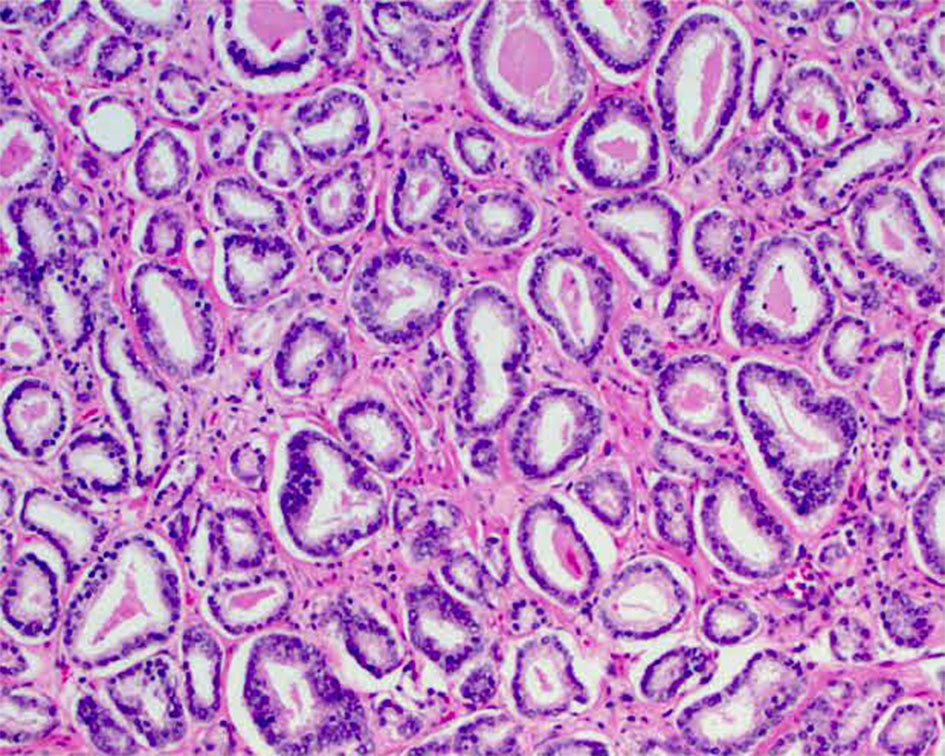
Figure 1. Gleason Score 3+3=6 (Grade Group 1) Adenocarcinoma (100x magnification).
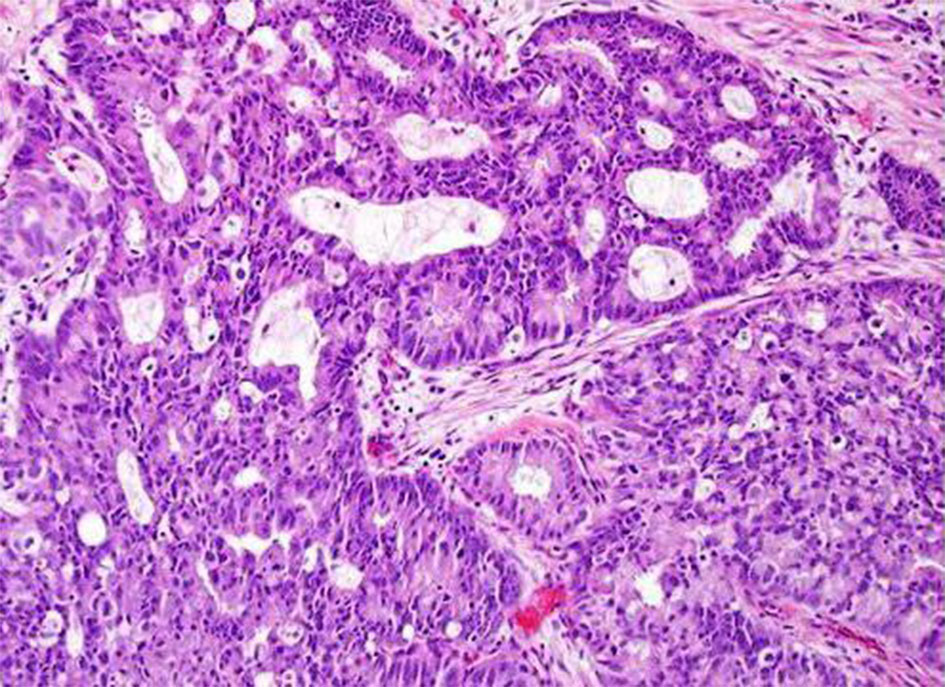
Figure 2. Gleason score 4+3=7 (Grade group 3) adenocarcinoma (100x magnification).
|
Table 1. Correlation of Serum PSA Test with Biopsy Results (n=100). |
|||
|
Ca prostate on Biopsy |
Present |
Absent |
Total |
|
Serum PSA > 4 ng/ml |
66 [TP] |
13 [FP] |
79 |
|
Serum PSA ≤ 4 ng/ml |
3 [FN] |
18 [TN] |
21 |
|
Total |
69 |
31 |
100 |
|
Table 2. Distribution of Serum PSA in Accordance with Gleason Score and Grade Groups (n=69). |
||||||
|
Serum PSA in ng/ml |
Group 1 [3 + 3 = 6] |
Group 2 [3 + 4 = 7] |
Group 3 [4 + 3 = 7] |
Group 4 [4 + 4 = 8] |
Group 5 [9-10] |
Total MalignantCases |
|
0 - 4 |
0 |
2 |
1 |
0 |
0 |
3 |
|
>4 - 10 |
2 |
3 |
2 |
1 |
1 |
9 |
|
>10 – 20 |
6 |
3 |
2 |
3 |
0 |
14 |
|
>20 – 50 |
5 |
4 |
4 |
1 |
3 |
17 |
|
>50 |
2 |
9 |
9 |
4 |
2 |
26 |
|
Total |
15 |
21 |
18 |
9 |
6 |
69 |
|
Table 3. Association between Prostate-specific antigen and Gleason score. |
|||||||
|
Gleason Score and Grade Groups (n=69) |
Serum PSA in ng/ml |
χ? |
Ρ |
||||
|
0 - 4 |
>4 - 10 |
>10 – 20 |
>20 – 50 |
>50 |
|||
|
Group 1 [3 + 3 = 6] |
0 |
2 |
6 |
5 |
2 |
15.569y |
0.065 |
|
Group 2 [3 + 4 = 7] |
2 |
3 |
3 |
4 |
9 |
||
|
Group 3 [4 + 3 = 7] |
1 |
2 |
2 |
9 |
4 |
||
|
Group 4 [4 + 4 = 8] |
0 |
1 |
3 |
1 |
4 |
||
|
Group 5 [9-10] |
2 |
9 |
9 |
4 |
2 |
||
|
y = chi-square. |
|
|
|
|
|
||
|
Table 4. Mean Serum PSA of each Gleason Grade Groups (n=69). |
|||||
|
|
Group 1 |
Group 2 |
Group 3 |
Group 4 |
Group 5 |
|
Gleason score |
3 + 3 = 6 |
3 + 4 = 7 |
4 + 3 = 7 |
4 + 4 = 8 |
9-10 |
|
Total no of patients |
15 |
21 |
18 |
9 |
6 |
|
Mean serum PSA |
21.3 ng/ml |
58.4 ng/ml |
73.6 ng/ml |
118.4 ng/ml |
96.3 ng/ml |
|
Table 5. Comparison of Serum PSA Distribution in Prostate Malignancy among Various Studies. |
||||
|
Studies |
Year |
Up to 4ng/ml |
4-10ng/ml |
>10ng/ml |
|
Our study |
2020 |
4.3% |
13% |
82.6% |
|
Wadgaonkar et al |
2013 |
- |
08% |
92% |
|
Zivkovic S et al |
2004 |
2.5% |
27.5% |
70% |
|
Xess et al |
2001 |
- |
16% |
74% |
|
Table 6. Correlation of Mean Serum PSA with Level of Differentiation in Prostate Malignancy among Various Studies. |
||||||||
|
Studies |
Year |
No. of Cases |
Well Differentiated |
ModerateDifferentiated |
PoorDifferentiated |
|||
|
% of total cases |
Mean PSA in ng/ml |
% of total cases |
Mean PSA in ng/ml |
% of total cases |
Mean PSA in ng/ml |
|||
|
Zivkovic S et al |
2004 |
40 |
17.5 |
7.9 |
52.5 |
22 |
30 |
41.5 |
|
Albashri A et al |
2014 |
65 |
5.6 |
100 |
41 |
210 |
36.6 |
588 |
|
Present study |
2020 |
69 |
- |
- |
78.2 |
51.1 |
21.8 |
107.3 |
Ninety per cent of the patients in our study presented with a poor stream, frequency, Nocturia and postvoid dribbling. Six patients presented with hematuria, and 4 patients with acute urinary retention. Obstructive LUTS in prostatomegaly is due to compression of the prostatic urethra. Aslamet al [12] and Raza et al [13] also found LUTS as the most common presenting symptom correlated with our study.
The majority of cancer patients in our study were in the 7th and 8th decade with a mean age of 71 years. Albashari A et al [14] studied 417 cases and observed 74 malignancy with a maximum number of patients falling in 70 - 89 years of age group with a mean age of 71.2 years, which was correlated with our study.
Malignancy of the prostate was seen in 69 (69%) patients in the present study. In our study, the Histomorphological spectrum of prostatic malignancy revealed adenocarcinoma as the commonest histological type of malignancy, accounting for 98.5% of cases. Jishaniet al [15] Mosli H et al [16] and Wadgaonkar et al [17] also had a similar observation.
Prostate adenocarcinoma approximately for the past 50 years has been graded by the system recommended by Donald F. Gleason [18]. In the present study, Gleason's score ranged from 6 to 10 with a predominance of score 6 and 7, which accounts for 54 patients out of 69 (78.2%) as also studied by Mosli et al17 and Shiris et al [19] with 57.7 per cent and 70.5 per cent cases respectively. As all the 100 patients underwent TRUS guided 16 core prostatic biopsy, a Gleason score of 2 to 4 and grade 1 to 2 is not assigned due to the limited amount of available biopsy tissue leading to a significant disparity study done by AZ Mohammad et al. [20]. The latter observed maximum cases with Gleason's score of 4.
PSA, a proteolytic enzyme, is produced by both normal and tumoral prostatic epithelium. A serum PSA level exceeding 4 ng/ml is abnormal and considered as a most sensitive marker for detection of prostate Carcinoma. However, this elevation is not specific to malignancy but may be due to benign prostatic hyperplasia, prostatitis, infarction and trauma (such as transurethral resection, needle biopsy) [3, 8].
In our study, 65 out of 69 patients [94.2%] with adenocarcinoma of prostate had serum PSA >4ng/ml. One patient had undifferentiated carcinoma of the prostate with a Gleason score of 5+5 and had a serum PSA of 7.02 ng/ml. Three patients with adenocarcinoma of the prostate have normal serum PSA. A study carried by ZivkovicS et al [21] showed 70% of their patients with adenocarcinoma had PSA values of more than 10ng/ml. They also found 2.5 % of patients had serum levels within normal limits. Similarly, another study by Xesset al [22] with 51 cases of adenocarcinoma shows most patients (74 per cent) have S.PSA levels of more than 10. Our present study is comparable to these studies (Table 5). Our study shows that serum PSA levels in patients with carcinoma prostate were widely distributed into three levels, normal (0-4ng/ml), intermediate (>4-10ng/ml) and high levels (>10ng/ml), and 57 out of 69 patients [82.6%] had serum PSA above 10ng/ml.
To correlate between Gleason's score with serum PSA levels, the patients were divided into 5 groups according to Gleason's score: Group 1 (score of 3+3=6), Group 2 (score of 3+4=7), Group 3 (score of 4+3=7), Group 4 (score of 4+4=8), Group 5 (score of 9-10). In our study, higher serum PSA levels were associated with higher Gleason score and grades.
The various Gleason scores were lumped together into three grade system-Well, moderately and poorly differentiated carcinoma, which corresponds to the Gleason score (2-4), Gleason score (5-7), Gleason score (8-10), respectively [23]. As this study included only patients undergoingTRUS guided biopsy, well-differentiated carcinoma is not assigned due to the limited amount of available biopsy tissue. Out of 69 patients, 54 patients (78.2%) were found to have moderate differentiation with mean serum PSA of 51.1ng/ml and 15 patients (21.8%) were found to have poor differentiation with mean serum PSA 107.3ng/ml. These results were compared with studies done by Zivkovic S et al. and Albashri A et al., respectively (Table 6).
The sensitivity and specificity of serum PSA in diagnosing prostate malignancy were found to be 95.6 and 58.0 in our study when the cut off for normal serum PSA is up to 4 ng/ml. Our study is comparable to Lakhey M et al. [24] and Shalini Agnihotriet et al [25]. They found 100% and 79% sensitivity, respectively, and specificity of 49% and 59%, respectively.
Nevertheless, one main limitation of our study is the relatively small sample size due to resource constraint; thus, large-scale randomized control trials are encouraged to be designed to verify the above results with increased statistical power.
Serum PSA is a highly sensitive tumor marker with a sensitivity of 95.6% and specificity of 58% in this study. Serum PSA has a low specificity as many benign and iatrogenic conditions also increases its level. It has a high negative predictive value which is important in ruling out malignancy. Digital rectal examination, transrectal ultrasonography and serum prostate specific antigen represents a diagnostic triad for the detection of prostatic carcinoma. In this study higher serum PSA levels were found to be correlated with higher Gleason score and grades. Mean serum PSA levels of moderately and poorly differentiated carcinoma were 51.1ng/ml and 107.3ng/ml respectively. Large-scale randomized control trials are encouraged to be designed to verify this conclusion with increased statistical power.
Acknowledgements
We extend their sincere thanks to all the patients who participated in the study.
Ethical policy
Approval from institutional ethical committee was taken, the principles of the Helsinki Declaration were followed.
Author contributions
VMR, Supervision, Critical Review; KO, Conception, Design, Materials, Data collection; EHG, Writing, Analysis and Interpretation; BR, Literature Review.
Competing interests
The authors declare no competing interests.
Funding
This study was financially not supported by any institution.
- American Cancer Society, 2017. Cancer facts and figures 2017. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/ cancer-facts-figures-2017.html.
- Siegel R, Ma J, Zou Z, Jemal A: Cancer statistics, 2014, CA Cancer J Clin 2014, 64(1): 9-29.
- Rosai J: Ackerman’s surgical pathology 19th ed. St. Louis U.S.A: Mosby Company 1989.
- Kumar V, Abbas AK, Fausto N, Aster J, editors: Robbins and Cotran Pathologic Basis of Disease, Professional Edition, 8th Edition.
- Gau JT, Salter RD, Krill D, Grove ML, Becich ML: The biosynthesis and secretion of prostate-specific antigen in LNCaP cells. Cancer Res 1997, 57(17): 3830-3834.
- Wang MC: Purification of a human prostate-specific antigen. Invest Urol 1979, 17(2): 159-163.
- Gleason DF, Mellinger GT: Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol 1974, 1(1): 58-64.
- Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL: ISUP Grading Committee: The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma, Am J SurgPathol 2005, 29(9): 1228-1242.
- Neal D: The prostate and seminal vesicles. In: Mann CV, Russel RCG, William NS, eds. Bailey and Love’s short practice of surgery. 22nd ed. Chapman Hall. London. 1995: 970-985.
- CalC, Gunaydin G, Ozyurt C, Omay S: Doxazosin: A new cytotoxic agent for prostate cancer. Br J Urol 2000, 85(6): 672-675.
- Iqbal N, Bhatti AN, Hussain S: Role of Digital Rectal Examination and prostate Specific Antigen in detecting carcinoma prostate. J Coll Physician Surg Pak 2003, 13(6): 340-342.
- Muhammad AH, Shahid N, Shaikh NA, Shaikh HA, Saleem S, Mughal A: Spectrum of prostatic lesions. Int Arch Med 2013, 6(1): 36.
- Raza I, Hassan N, Jafri A, Gul P: Relationship between Benign Prostatic Hyperplasia and International Prostatic Symptom Score. Br J Med Med Res 2015, 10(5): 1-9.
- Albasri A, El-Siddig A, Hussainy A, Mahrous M, Alhosaini AA, Alhujaily A: Histopathologic Characterization of Prostate Diseases in Madinah, Saudi Arabia. Asian Pac J Cancer Prev 2014, 15(10): 4175-4179.
- Jasani JH, Patel HB, Gheewala B, Vaishnavi HV, Bhuva K, Sancheti S: Diagnostic utility of prostate-specific antigen for detection of prostatic lesions. Int J Biomed Adv Res 2012, 3(4): 268-272.
- Most HA, Abdel-Meguid TA, Al-Maghrabi JA, Kamal WK, Saadah HA, Farsi HM: The clinicopathologic patterns of prostatic diseases and prostate cancer in Saudi patients. Saudi Med J 2009, 30(11): 1439-1482.
- Wadgaonkar: Correlation of serum prostate-specific antigen (PSA) level in various prostate pathology in elderly men. Int J Basic Appl Med Sci 2013, 3(2): 274-281.
- Brimo F, Vollmer RT, Corcos J, Kotar K, Begin LR, Humphrey PA, Bismar TA: Prognostic value of various morphometric measurements of tumour extent in prostate needle core tissue. Histopathology 2008, 53(2): 177-183.
- Shirish C, Jadhav PS, Anwekar SC, Kumar H, Buch AC, Chaudhari US: Clinicopathological study of benign and malignant lesion of the prostate. Int J Pharm BiolSci 2013, 3(1): 162-178.
- Mohammed AZ, Alhassan SU, Edino ST, Ochicha O: Histopathological review of prostatic diseases in Kano Nigeria. Niger Postgrad Med J 2003, 10(1): 1-5.
- Zivkovic S: Correlation prostate-specific antigen and histopathological difference of prostate carcinoma. Arch Oncol 2004, 12(3): 148-151.
- Xess A, Singh M, Raghwendra KH, Sharma HP, Shahi SK: PSA as a tumour marker; relationship with histological grading. Indian J PatholMicrobiol 2001, 44(3): 261-264.
- Ali A: Significance of Gleason system for grading and scoring of prostatic carcinoma. Pak J Med Res 2004, 43(4).
- Lachey M, Ghimire R, Shrestha R, Bhatta AD: Correlation of serum-free prostate-specific antigen level with histological findings in patients with prostatic disease. Kathmandu Univ Med J 2010, 8(30): 158-163.
- Agnihotri S, Mittal RD, Kapoor R, Mandhani A: Raising cut-off value of prostate-specific antigen (PSA) for biopsy in symptomatic men in India to reduce unnecessary biopsy. Indian J Med Res 2014, 139(6): 851-856.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript