Case Report | Open Access
Exploring Scrotal Leiomyomas, Unraveling the Mysteries of a Rare Tumor: A Case Report
Sana Ahuja1, Pooja Verma1, Adil Aziz Khan1, Sufian Zaheer1
1Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
Correspondence: Sufian Zaheer (Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, Ansari Nagar, New Delhi, India; Email: sufianzaheer@gmail.com).
Annals of Urologic Oncology 2024, 7(1): 43-47. https://doi.org/10.32948/auo.2024.01.28
Received: 22 Jan 2024 | Accepted: 28 Jan 2024 | Published online: 30 Jan 2024
Key words scrotal, leiomyoma, sebaceous cyst, mesenchymal
A 48-year-old male presented with a painless lump on the right side of the scrotum persisting for the past 9 months. Upon physical examination, a firm, non-tender, mobile, and round lump measuring 1.5 cm × 1.5 cm × 1 cm was identified at the root of the right scrotum, distinct from the testes. The overlying skin appeared normal, and no palpable inguinal lymph nodes were observed. Clinically, the lump was preliminarily diagnosed as a papilloma. Subsequently, it was excised and submitted for histopathological evaluation.
The gross examination revealed a single, partially skin-covered, grey-brown soft tissue piece measuring 1.5 cm × 1.5 cm × 0.8 cm. The cut surface exhibited a solid, and homogeneous tumor with whorling.
Microscopic examination unveiled a stratified squamous epithelial-lined tissue. In the subepithelium, a well-circumscribed tumor comprised interlacing bundles of smooth muscles with varying amounts of admixed collagen, displaying hyaline degeneration. Individual muscle cells exhibited uniform size and shape, with oval to spindle nuclei and bipolar cytoplasm. No cytological atypia or increased mitotic figures was observed. Immunohistochemistry indicated positive expression for vimentin, desmin and smooth muscle actin (SMA). Ki67 proliferation index was 2-3% (Figure 1).
The final diagnosis was confirmed as scrotal leiomyoma. The post-operative period was uneventful with no complications/ recurrence till date.
Case 2
A 25-year-old man presented with complaints of scrotal swelling persisting for the past year. Upon physical examination, a firm, non-tender, mobile, round lump measuring 2 cm × 1.5 cm × 1 cm was identified on the right side of the scrotum. The lump exhibited no palpable connection to the testes, epididymis, or spermatic cord. The overlying skin appeared normal without any ulceration, and both testes were normal, with no palpable inguinal lymph nodes. Clinically, the scrotal lump was diagnosed as an epidermal inclusion cyst. The swelling was excised and submitted for histopathological examination.
The gross examination of the scrotal swelling revealed a single, partially skin-covered, grey-brown soft tissue piece measuring 1.5 cm × 1.5 cm × 0.8 cm. The cut surface appeared solid, and homogeneous, and displayed a whorling pattern.
Microscopic examination of the scrotal swelling revealed stratified squamous epithelial-lined tissue. The subepithelium exhibited a well-circumscribed tumor composed of interlacing bundles of smooth muscles with varying amounts of admixed collagen. Individual muscle cells were uniform in size and shape, with oval to spindle nuclei and bipolar cytoplasm. No evidence of cytological atypia or mitotic figures was observed. Immunohistochemistry results indicated positivity for vimentin, desmin, and SMA (Figure 2). Ki67 proliferation index was 1-2%. The histopathological features were consistent with scrotal leiomyoma.
The post-operative period was uneventful with no complications/ recurrence till date.
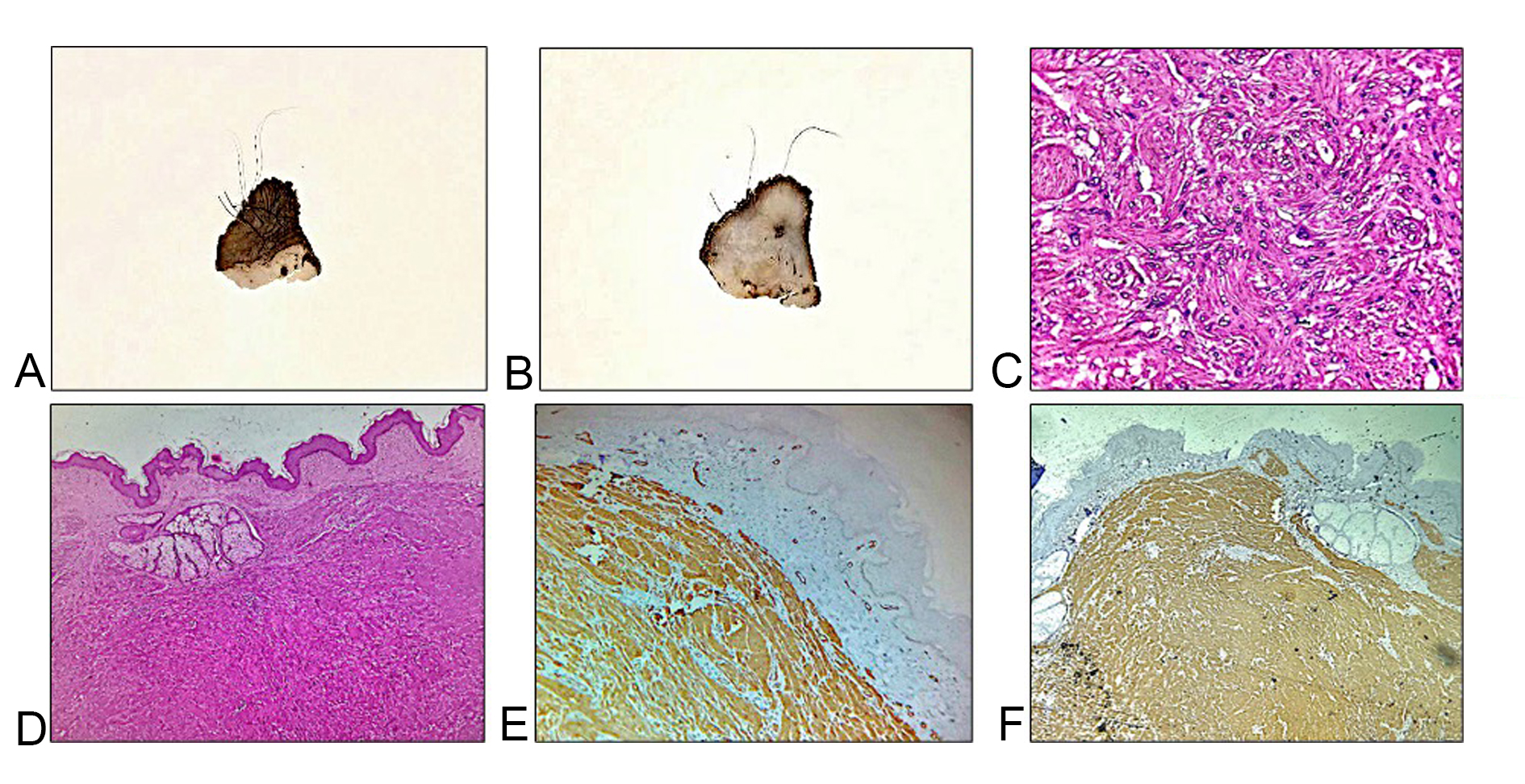 Figure 1. Gross and photomicrographs of Case 1. (A, B) Gross images show a homogeneous grey white solid tumor lying below the scrotal skin; (C, D) Hematoxylin and eosin stained sections show a well-circumscribed tumor with interlacing bundles of spindle shaped cells (40x, 400x magnification); (E, F) Immunohistochemical examination exhibited positive cytoplasmic expression for desmin and smooth muscle actin (40x magnification).
Figure 1. Gross and photomicrographs of Case 1. (A, B) Gross images show a homogeneous grey white solid tumor lying below the scrotal skin; (C, D) Hematoxylin and eosin stained sections show a well-circumscribed tumor with interlacing bundles of spindle shaped cells (40x, 400x magnification); (E, F) Immunohistochemical examination exhibited positive cytoplasmic expression for desmin and smooth muscle actin (40x magnification).
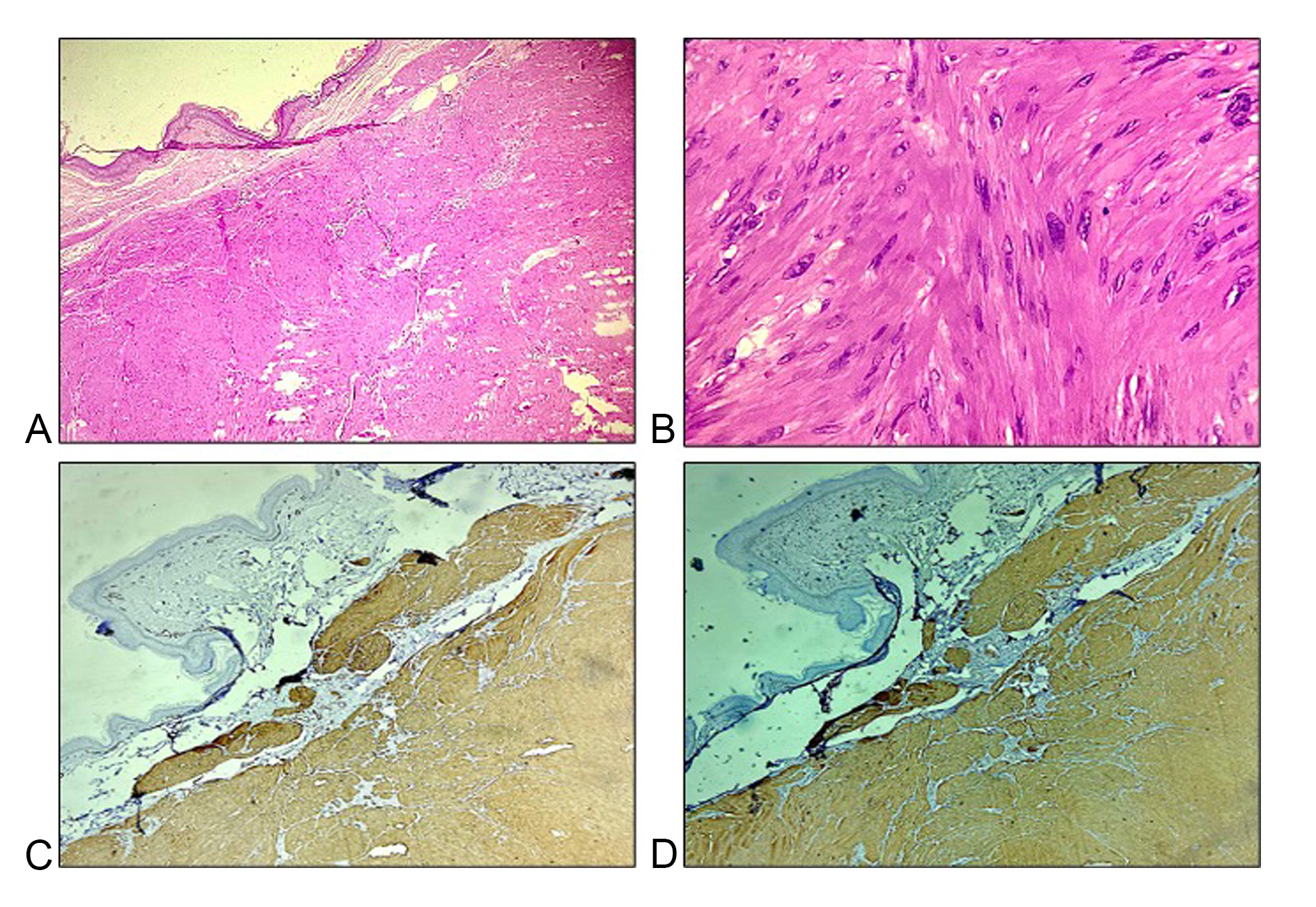 Figure 2. Histopathological and immunohistochemical images of Case 2. (A, B) Hematoxylin and eosin stained sections show a well-circumscribed tumor with interlacing bundles of spindle-shaped cells (40x, 400x magnification); (C, D) Immunohistochemical examination exhibited positive cytoplasmic expression for desmin and smooth muscle actin (40x magnification).
Figure 2. Histopathological and immunohistochemical images of Case 2. (A, B) Hematoxylin and eosin stained sections show a well-circumscribed tumor with interlacing bundles of spindle-shaped cells (40x, 400x magnification); (C, D) Immunohistochemical examination exhibited positive cytoplasmic expression for desmin and smooth muscle actin (40x magnification).
Scrotal smooth muscle tumors are classified into leiomyoma, atypical leiomyoma, and leiomyosarcoma. Four pathological criteria are utilized to grade scrotal smooth muscle cell tumors, including size ≥ 5cm in greatest dimension, infiltrative margin, ≥5 mitotic figures per 10 high power fields, and moderate cytological atypia. Tumors meeting only one criterion are deemed benign, those fulfilling two criteria are considered atypical leiomyoma, and those demonstrating three or four criteria are classified as leiomyosarcoma.
Previously, Adil et al. (2021) reported a case of scrotal leiomyoma in an 82-year-old male with a left scrotal mass persisting for 3 years. Imaging studies revealed a left paratesticular mass, and surgery confirmed the histopathological features consistent with scrotal leiomyoma [12]. Egharevba et al. (2020) also presented a case of scrotal leiomyoma in a 39-year-old male with a progressive right-sided hemiscrotal swelling over one year, which was excised, and histopathology revealed scrotal leiomyoma [13]. Table 1 summarizes the previously reported cases of scrotal leiomyoma.
Accurate diagnosis is crucial for guiding appropriate management strategies. Clinicians often employ a combination of clinical evaluation, imaging studies, and histopathological examination to confirm the presence of scrotal leiomyomas. Ultrasound remains a valuable tool for assessing the size, location, and vascularity of the tumor, aiding in the formulation of a differential diagnosis. Definitive diagnosis, however, relies on histological examination, which typically reveals spindle-shaped smooth muscle cells arranged in interlacing bundles.
Clinical manifestations of scrotal leiomyoma may lack distinctive characteristics, with a clinical differential diagnosis including sebaceous cysts, fibromas, adnexal tumors, neurofibromas, schwannomas (if painful), and squamous cell carcinoma (if ulcerated) [8, 14]. If there is any adhesion to the testis, consideration should be given to the possibility of atypical leiomyoma or leiomyosarcoma. Surgical excision stands as the primary treatment for scrotal leiomyomas. Complete excision is generally curative, with a low rate of recurrence reported in the literature. Minimally invasive techniques, such as laparoscopy or sclerotherapy, have shown promising results in select cases. However, the optimal approach may vary based on the size and location of the tumor, as well as the patient's overall health. Long-term follow-up is essential to monitor for recurrence and assess the overall prognosis [3].
Given the limited number of reported cases and the paucity of large-scale studies, scrotal leiomyomas remain an enigmatic entity in the realm of genitourinary tumors. Further research is warranted to elucidate the underlying molecular mechanisms, explore potential biomarkers for early detection, and refine treatment algorithms. Collaborative efforts among researchers and clinicians will be instrumental in creating a comprehensive understanding of scrotal leiomyomas and improving patient outcomes.
|
Table 1. Previously reported cases of scrotal leiomyoma. |
|||||
|
Author |
Age |
Clinical presentation |
Clinical differential |
Radiological findings |
Final diagnosis |
|
Rana et al (2015) [1] |
75 |
Painless mass right side of scrotum |
Sebaceous cyst |
- |
Scrotal leiomyoma |
|
Aluko et al (2018) [2] |
37 |
Painless right scrotal mass |
Lipoma/ adenomatoid tumor/ papillary cystadenoma/ leiomyoma |
USG: A 5.2-cm hypoechoic vascular mass within the right scrotal sac |
Scrotal leiomyoma |
|
Ariafar et al (2020) [3] |
71 |
Left testicular enlargement and heaviness |
- |
USG: Scrotal mass |
Scrotal leiomyoma |
Fakhralddin et al (2020) [4]
|
52 |
Painless lump, scrotum |
- |
USG: 40 mm × 20 mm hypoechoic, poorly vascular lesion in the scrotum |
Scrotal leiomyoma |
|
Su et al (2014) [5] |
53 |
Painless right scrotal mass |
Sebaceous cyst |
- |
Bizzare leiomyoma |
|
Asotra et al (2016) [6] |
50 |
Painless left scrotal mass |
Sebaceous cyst |
- |
Scrotal leiomyoma |
|
Bell et al (2016) [7] |
47 |
Mildly painful, slowly enlarging nodule on his left hemiscrotum |
Sebaceous cyst |
USG: 7 mm superficial, hypoechoic soft-tissue nodule |
Scrotal leiomyoma |
|
Patel et al (2019) [8] |
71 |
Painless left scrotal mass |
- |
- |
Scrotal leiomyoma |
|
Makkapati et al (2024) [9] |
55 |
Painless right scrotal mass |
Sebaceous cyst |
- |
Scrotal leiomyoma |
|
Wang et al (2023) [10] |
53 |
Constant heaviness in the right scrotum |
- |
USG: Well-circumscribed and heterogenous hypoechoic tumor |
Scrotal leiomyoma |
|
Sherwani et al (2008) [11] |
50 |
Painless left scrotal mass |
Sebaceous cyst |
- |
Scrotal leiomyoma |
|
Adil et al (2021) [12] |
82 |
Left scrotal enlargement |
- |
USG: 7 × 4cm, intra-scrotal extra-testicular well-circumscribed mass, with mixed, heterogeneous echogenicity |
Scrotal leiomyoma |
|
Egharevba et al (2020) [13] |
39 |
Right hemiscrotal swelling |
Epidermoid cyst, adenomatoid tumor |
USG: 4.9 cm × 3.9 cm well-circumscribed mass with mixed echogenicity attached to the lower pole of the right testis |
Scrotal leiomyoma |
|
Li et al (2013) [14] |
32 |
Painless right scrotal mass |
- |
- |
Scrotal leiomyoma |
Not applicable.
Ethical policy
Informed patient consent was taken. Any identifying details (such as name, date of birth) of the patient will not be published.
Availability of data and materials
That data is available from the corresponding author on request.
Author contributions
All authors contributed to the study conception and design.Material preparation, data collection and analysis were performed by Pooja Verma, Sana Ahuja, Adil Aziz Khan and Sufian Zaheer. The first draft of the manuscript was written by Pooja Verma and Sana Ahuja and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors have no conflicts of interest to declare.
Funding
None.
- Rana S, Sharma P, Singh P, Satarkar RN: Leiomyoma of Scrotum: a Rare Case Report. Iran J Pathol 2015, 10(3): 243-247.
- Aluko T, Masi Z, Tomaszewski J, Germaine P: Scrotal sac leiomyoma: Case report of a rare benign scrotal mass. Radiol Case Rep 2018, 13(2): 411-414.
- Ariafar A, Soltani M, Khajeh F, Zeighami S, Naghdi Sedeh N, Miladpour: Scrotal leiomyoma a rare benign intra-scrotal mass could lead to unnecessary orchiectomy. Urol Case Rep 2020, 32: 101170.
- Fakhralddin SS, Bapir R, Babarasul MH, Ibrahim ZB, Aghaways I: Typical leiomyoma of the scrotum: A rare case report. Int J Surg Case Rep 2020, 67: 142-145.
- Su Z, Li G, Wang Y, Yu Z, Chen Z, Ni L, Yang S, Ye J, Lai Y: Bizarre leiomyoma of the scrotum: A case report and review of the literature. Oncol Lett 2014, 7(5): 1701-1703.
- Asotra S: Leiomyoma of scrotum. Arch of Med He Sci 2016, 4: 238-240.
- Bell RC, Austin ET, Arnold SJ, Lin FC, Walker JR, Larsen BT: Rare leiomyoma of the tunica dartos: A case report with clinical relevance for malignant transformation and HLRCC. Case Rep Pathol 2016, 2016: 6471520.
- Patel H, Patel N: Leiomyoma of scrotum: A case report of a common benign tumor at a rare site. Int J Clin Diagn Pathol 2019, 2: 261-262.
- Makkapati S, Venkatasubramanian R, Muralidharan M: Rare case of a scrotal leiomyoma-a diagnostic dilemma: A case report. Int J Surg Case Rep 2024, 114: 109178.
- Wang P: Scrotal Leiomyoma: A Case Report of a Rare Intra-Scrotal Benign Mass. Cur Med Imaging 2023, 19(8): 962-964.
- Sherwani RK, Rahman K, Akhtar K, Zaheer S, Hassan MJ, Haider A: Leiomyoma of scrotum. Indian J Pathol Microbiol 2008, 51(1): 72-73.
- Adil H, Mrabti M, Semedo A, El Fenni J, Abdellaoui M: Scrotal leiomyoma: An uncommon cause of chronic scrotal swelling. Radiol Case Rep 2021, 16(8): 2787-2791.
- Egharevba PA, Omoseebi O, Okunlola AI, Omisanjo OA: Scrotal leiomyoma: a rare cause of scrotal swelling. Afr J Urol 2020, 26: 1-4.
- Li SL, Han JD: A case report of atypical scrotal leiomyoma. Case Rep Dermatol 2013, 5(3): 316-320.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript