Case Report | Open Access
Multilocular Cystic Renal Neoplasm of Low Malignant Potential: Mimicker of Cystic Clear Cell Carcinoma – Urologist’s Perspective
Harish Challa1, Hariharasudhan Sekar2, Sandhya Sundaram3, Sriram Krishnamoorthy4, Natarajan Kumaresan4
1Department of Urology, Sri Ramachandra Institute of Higher Education & Research, Porur, Chennai 600116, India.
2Department of Urology, Sri Ramachandra Institute of Higher Education & Research, Porur, Chennai 600116, India.
3Department of Pathology, Sri Ramachandra Institute of Higher Education & Research, Porur, Chennai 600116, India.
4Department of Urology, Sri Ramachandra Institute of Higher Education & Research, Porur, Chennai 600116, India.
Correspondence: Sriram Krishnamoorthy (Department of Urology and Renal transplantation, Sri Ramachandra Institute of Higher Education & Research Porur, Chennai 600116; Email: sriramuro@gmail.com).
Annals of Urologic Oncology 2020, 3(1): 22-26. https://doi.org/10.32948/auo.2020.12.09
Received: 13 Nov 2020 | Accepted: 06 Dec 2020 | Published online: 31 Dec 2020
Case report A 46-year-old male presented with continuous mild loin pain for a month. There were no lower tract urinary symptoms. Ultrasound abdomen showed left lower pole renal mass. CECT-KUB was done as a definitive investigation which showed a solitary left lower pole renal cystic lesion with enhancement of size 3.8x3.6cm (Bosniak IV). As per CT findings, the patient underwent Laparoscopic partial nephrectomy. Histopathological examination showed multiple cysts with thin septal walls possessing clear cells with low-grade nuclei. 2 years of follow-up postoperatively with imaging studies revealed no recurrence or metastasis.
Conclusions The purpose of this report is to emphasize the need to identify this entity by strict histological criteria as per WHO guidelines, as imaging studies were more often inconclusive. Urologists should have an adequate understanding such an entity. Almost all cases are amenable to partial nephrectomy irrespective of size and no documented evidence of recurrence and metastasis which mandates less stringent follow up postoperatively as compared to ccRCC.
Key words kidney, tumour, nephroma, cystic carcinoma, nephrectomy
Multilocular cystic renal cell carcinoma (MCRCC) is a very rare subtype of clear cell renal cell carcinoma (CCRCC) accounting for 2-4% of CCRCC. It is a purely cystic kidney tumour that has cellular features and cytogenetic alterations (3p mutation, VHL) that are virtually identical to that of CCRCC [1, 2].
Recently, the International Society of Urological Pathology (ISUP 2013) and the World Health Organization (WHO 2016) redesignated the classification of tumours of the kidney [3-5]. Because of distinct pathological patterns and no incidence of recurrence and metastasis, MCRCC was redesignated as Multilocular cystic renal neoplasm of low malignant potential (MCRNLMP) [6].
WHO proposed relatively strict diagnostic criteria and defined MCRNLMP as "a neoplasm that is composed entirely of numerous cysts surrounded by a fibrous capsule and septa that contains clear cells without expansile growth or mural nodules" (WHO 2016). These tumours are morphologically and radiologically indistinguishable from low-grade cystic CCRCC.
ISUP (2013) replaced the term “carcinoma” to low malignant potential [7, 8]. Tretiakova et al., [9] summarized from all similar sources available in the literature and concluded that MCRNLMP patients with atleast five-year follow-up had no recurrence or metastasis. The purpose of this manuscript is to emphasize the importance of identifying these entities by strict histological criteria as defined by WHO (2016) and making the urologists aware of this potentially curable condition. These lesions fall under the lower risk category, irrespective of TNM staging. On long term follow-up, as compared to CCRCC, there are no documented cases of recurrence or metastasis noted after complete resection by either radical or partial nephrectomy [10].
A 46-year-old non-smoker male presented with continuous dull aching left loin pain for one-month duration. He did not have any bothersome lower urinary tract symptom or any medical comorbidities. His blood biochemical investigations, renal and liver function tests were normal.
Ultrasonography of the whole abdomen showed a left lower pole cystic renal mass. Contrast-enhanced computed tomography (CECT KUB) scan showed a well defined, solitary, partially exophytic mass that was multicystic with solid components within them (Bosniak Category – IV). It was heterogeneously enhancing left lower pole renal mass, measuring 3.8X3.6cm (Figure 1). The patient underwent laparoscopic partial nephrectomy. Postoperative period was uneventful.
Gross examination of the specimen showed a single lesion of size 4.2x3 cm, encapsulated, purely multicystic possessing varying sizes of non-communicating cysts with clear serous or gelatinous material as content. There was no necrosis or solid nodules. Microscopic examination showed a multicystic lesion with thin septal walls of fibro-collagenous connective tissue containing single or occasionally multiple layers of clear cuboidal cells containing abundant cytoplasm (Figure 2A, 2B).These cells had small hyperchromatic nuclei with regular borders and inconspicuous or absent nucleoli (ISUP grade 1 - low grade). Mitotic figures were scarce. No expansile mural nodules, necrosis, vascular invasion, hyalinization or sarcomatoid changes were noted. Immunohistochemistry showed strong membrane positivity for vimentin and epithelial membrane antigen (EMA) (Figure 3A, 3B). Tumour falls under T1bN0M0 with ISUP nuclei grade 1. The patient is on regular follow-up with imaging studies and has a disease-free survival of more than three years.
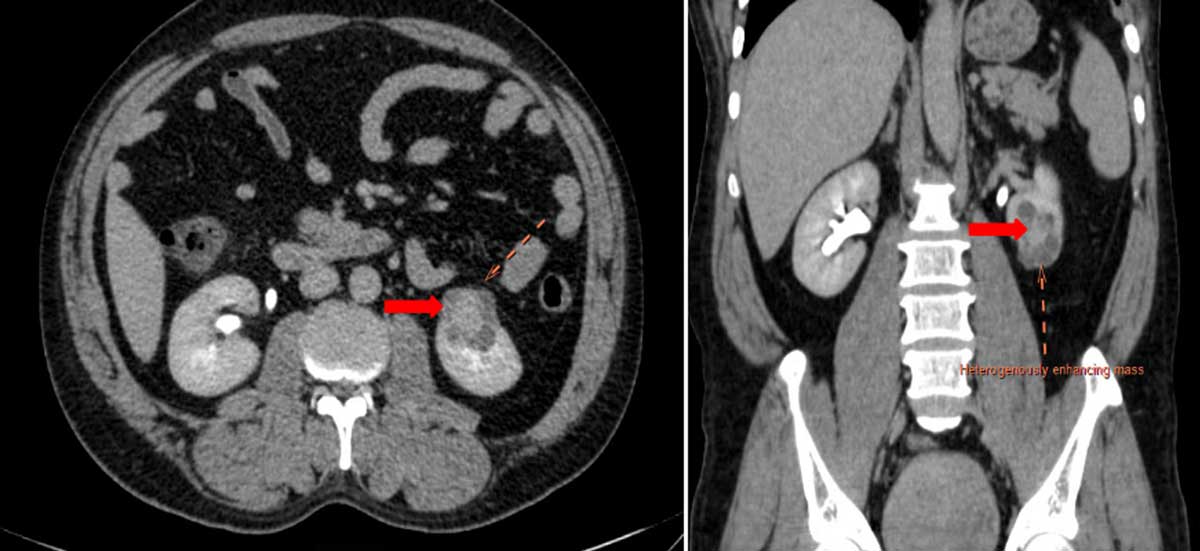 Figure 1. Contrast enhanced CT-KUB showing a well defined, solitary, partially exophytic, multicystic with solid component, heterogeneously enhancing left lower pole renal mass.
Figure 1. Contrast enhanced CT-KUB showing a well defined, solitary, partially exophytic, multicystic with solid component, heterogeneously enhancing left lower pole renal mass.
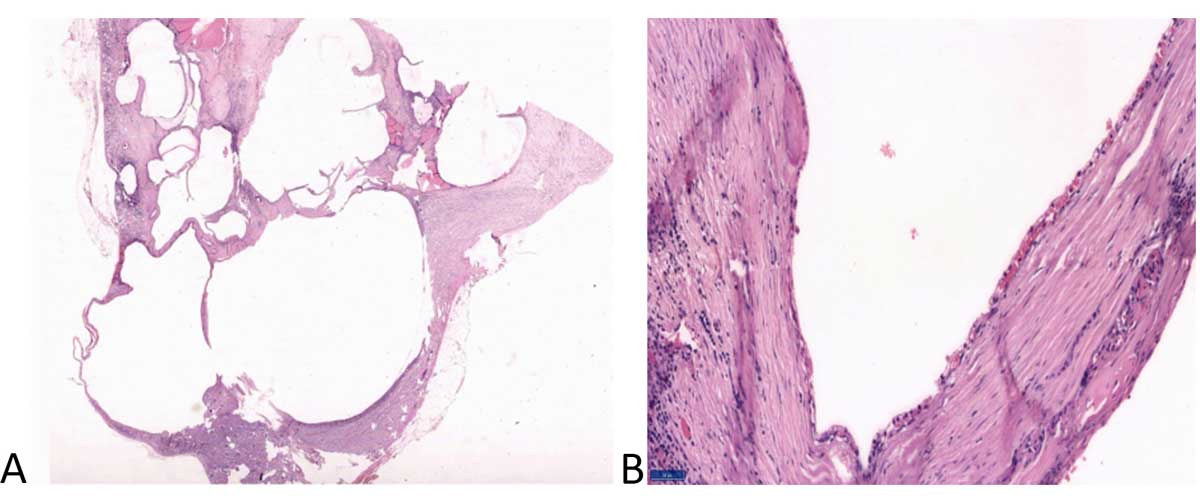 Figure 2. Haematoxylin & Eosin staining of the cystic lesion. (A) Multiple cystically dilated spaces separated by thin fibrous septae (20X); (B) Cystic spaces are lined by a single layer of low cuboidal epithelial cells with clear cytoplasm (100X).
Figure 2. Haematoxylin & Eosin staining of the cystic lesion. (A) Multiple cystically dilated spaces separated by thin fibrous septae (20X); (B) Cystic spaces are lined by a single layer of low cuboidal epithelial cells with clear cytoplasm (100X).
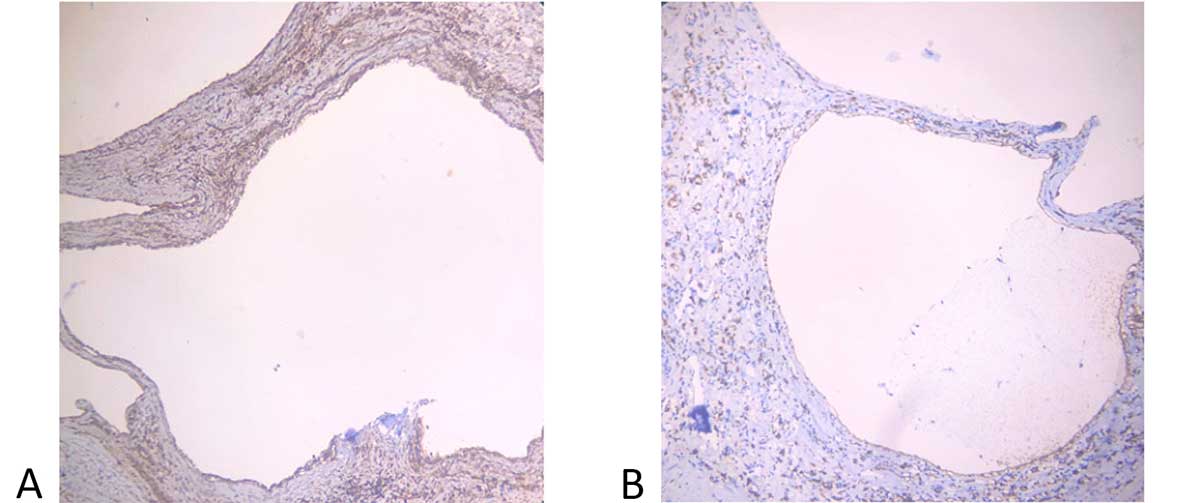 Figure 3. Immunohistochemistry of the tumour showing positivity for vimentin (A) and EMA (B) staining in the cystic lining cells (Immunostains, X100).
Figure 3. Immunohistochemistry of the tumour showing positivity for vimentin (A) and EMA (B) staining in the cystic lining cells (Immunostains, X100).
The term MCRNLMP was first suggested by Suzigan et al. [14] in 2006, where they revisited 2004 WHO classification of renal tumours. In his study on 45 patients with multilocular cystic RCC, they observed that the condition carried an excellent prognosis and the five-year disease-specific survival rate was 100%. They observed that 82% of their cases in were T1 stage and the low nuclear grade was found in 100% cases (G1-62% and G2-38%). In their series, none of the patients had any evidence of disease after surgery.
The term MCRCC was renamed as MCRNLMP by ISUP in 2013. The WHO Classification of 2016 as well subsequently accepted this change in terminology. MCRNLMP is de?ned as a multilocular cystic tumour lined by low ISUP grade (1-2) clear cells, immunohistochemically and molecularly not different from CCRCC [15].
It would be of some clinical significance, had any of the imaging studies given guidelines to differentiate atypical renal cysts, partially cystic RCC and MCRNLMP [16]. All three conditions look similar in imaging that prevents a Urologist or Radiologist in diagnosing this condition pre-operatively. However, histopathological examination could clearly distinguish between the three types. The gross features included well-encapsulated multilocular non-communicating cysts containing clear serous or gelatinous fluid or rarely hemorrhagic debris but absent solid nodules or tumour necrosis [17]. The microscopic features include cysts with septae lined by clear cuboidal cells with low-grade nuclei either as a single layer or in aggregates. A lack of expansile growth or solid nodules is a characteristic finding in such conditions [18]. Immunohistochemistry is positive for CD10, EMA and vimentin.
Other primary differential diagnoses include cystic nephroma, cystic clear cell papillary RCC and tubulocystic RCC [19]. Cystic nephroma is seen predominantly in females, and the presence of ovarian type stroma is a distinguishing factor. Cystic clear cell papillary RCC also contains clear cells with low-grade nuclei, but differentiating feature is the presence of papillary architecture. Tubulocystic RCC lining cells have eosinophilic cytoplasm with high-grade nuclei instead of clear cells. As described earlier, the differentiating factor for cystic CCRCC is the presence of expansile nodules.
Li et al., [20] in one of the most extensive reported case series of 76 patients concluded that these tumours were predominantly of a low nuclear grade irrespective of tumour size and TNM staging and suggested longer follow-up interval to minimize unnecessary investigations. Nassir et al. [21] defined MCRNLMP as a predominantly cystic lesion with neoplastic clear cells, probably a subtype of CCRCC having a benign clinical course.
Gong et al., [22] in their study on 31 patients, found that Multilocular cystic RCC had no tumour progression or metastasis and had excellent prognosis. Murad et al. [23] in one of the most extended follow-up of 6 cases of MCRNLMP observed neither recurrence nor metastasis concluding that these tumours are a low-grade variant of RCC with excellent prognosis.
A comparative study between MCRNLMP and predominantly cystic CCRCC by Tretiakova et al. [9] concluded MCRNLMP had uniformly good behavior and support ISUP recommendation for its non-carcinoma designation. They also concluded that predominantly cystic CCRCC had better prognosis as compared to solid or non-cystic CCRCC and the extent of the cystic component should be mentioned in the histopathology report by the reporting pathologist.
These studies confirmed that MCRNLMP is a low grade, well-defined tumour and most cases were amenable to partial nephrectomy with no recurrence and metastasis. In our case, on three years follow-up post partial nephrectomy with annual clinical examination and imaging studies, showed no recurrence or metastasis. Urologists should have an adequate understanding of this entity because we can adopt longer follow-up intervals for patients with this tumour to minimize unnecessary examinations and patient anxiety.
Acknowledgements
NIL
Ethical policy
Approval was taken from institutional ethical committee. The study was performed in accordance with the Declaration of Helsinki. Patients gave their informed consent for their participation.
Author contributions
All authors have equally contributed to the manuscript.
Competing interests
NIL
Funding
NIL
- Teichman A, Compérat E, Behnke S, Storz M, Moch H, Schraml P: VHL mutations and dysregulation of pVHL- and PTEN-controlled pathways in multilocular cystic renal cell carcinoma. Modern Pathology 2010, 24(4): 571-578.
- Grignon DJ, Bismar TA, Bianco F: VHL gene mutations in multilocular cystic renal cell carcinoma: evidence in support of its classification as a type of clear cell renal cell carcinoma. Mod Pathol 2004, 17 (suppl1): 154A.
- Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, Hes O, Moch H, Montironi R, Tickoo SK, et al: The International Society of Urological Pathology (ISUP) vancouver classification of renal neoplasia. Am J Surg Pathol 2013, 37(10): 1469-1489.
- International Agency for Research on Cancer: WHO Classification of Tumours of the Urinary System and Male Genital Organs. 2016, ISBN: 9789283224372.
- Moch H, Humphrey PA, Ulbright TM, Reuter VE: WHO classification of tumours of the urinary system and male genital organs, 4th edn. Lyon, France. 2016.
- Montironi R, Mazzucchelli R, Scarpelli M, Lopez-Beltran A, Cheng L: Update on selected renal cell tumors with clear cell features. With emphasis on multilocular cystic clear cell renal cell carcinoma. Histopathology 2013, 28(12): 1555-1566
- Hes O: International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia 2012 [International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia 2012].
- Kristiansen G, Delahunt B, Srigley JR, Lüders C, Lunkenheimer JM, Gevensleben H, Thiesler T, Montironi R, Egevad L: [Vancouver classification of renal tumors: Recommendations of the 2012 consensus conference of the International Society of Urological Pathology (ISUP)]. Pathologe 2015, 36(3): 310-316.
- Tretiakova M, Mehta V, Kocherginsky M, Minor A, Shen SS, Sirintrapun SJ, Yao JL, Alvarado-Cabrero I, Antic T, Eggener SE, et al: Predominantly cystic clear cell renal cell carcinoma and multilocular cystic renal neoplasm of low malignant potential form a low-grade spectrum. Virchows Arch 2018, 473(1): 85-93.
- Bhatt JR, Jewett MA, Richard PO, Kawaguchi S, Timilshina N, Evans A, Alibhai S, Finelli A: Multilocular cystic renal cell carcinoma: pathological T staging makes no difference to favorable outcomes and should be reclassified. J Urol 2016, 196: 1350-1355.
- Chang CC, Kuo JY, Chan WL, Chen KK, Chang LS: Prevalence and clinical characteristics of simple renal cyst. J Chin Med Assoc 2007, 70(11): 486-491.
- Hartman DS, Davis CJ Jr, Johns T, Goldman SM: Cystic renal cell carcinoma. Urology 1986, 28(2): 145-153.
- Halat S, Eble JN, Grignon DJ, Lopez-Beltran A, Montironi R, Tan PH, Wang M, Zhang S, MacLennan GT, Cheng L: Multilocular cystic renal cell carcinoma is a subtype of clear cell renal cell carcinoma. Mod Pathol 2010, 23(7): 931-936.
- Suzigan S, López-Beltrán A, Montironi R, Drut R, Romero A, Hayashi T, Gentili AL, Fonseca PS, deTorres I, Billis A, et al: Multilocular cystic renal cell carcinoma: a report of 45 cases of a kidney tumor of low malignant potential. Am J Clin Pathol 2006, 125(2): 217-222.
- Montironi R, Lopez-Beltran A, Cheng L, Scarpelli M: Words of wisdom: re: multilocular cystic renal cell carcinoma with focus on clinical and pathobiological aspects. Eur Urol 2013, 63(2): 400-401.
- Aubert S, Zini L, Delomez J, Biserte J, Lemaitre L, Leroy X: Cystic renal cell carcinomas in adults. Is preoperative recognition of multilocular cystic renal cell carcinoma possible? J Urol 2005, 174(6): 2115-2119.
- Mazzucchelli R, Scarpelli M, Montironi R, Cheng L, Lopez Beltran A: Multilocular cystic renal cell neoplasms of low malignant potential. Anal Quant Cytopathol Histopathol 2012, 34(5): 235-238.
- Williamson SR, MacLennan GT, Lopez-Beltran A, Montironi R, Tan PH, Martignoni G, Grignon DJ, Eble JN, Idrees MT, Scarpelli M, et al: Cystic partially regressed clear cell renal cell carcinoma: a potential mimic of multilocular cystic renal cell carcinoma. Histopathology 2013, 63(6): 767-779.
- Ebin JN, Bonsib SM: Extensively cystic renal neoplasms: Cystic nephroma, cystic partially differentiated nephroblastoma, multilocular cystic renal cell carcinoma and cystic hamartoma of renal pelvis. Semin Diagn Pathol 1998, 15(1): 2-20.
- Li T, Chen J, Jiang Y, Ning X, Peng S, Wang J, He Q, Yang X, Gong K: Multilocular Cystic Renal Cell Neoplasm of Low Malignant Potential: A Series of 76 Cases. Clin Genitourin Canc 2016, 14(6): e553-e557.
- Nassir A, Jollimore J, Gupta R, Bell D, Norman R: Multilocular cystic renal cell carcinoma: a series of 12 cases and review of the literature. Urology 2002, 60(3): 421-427.
- Gong K, Zhang N, He Z, Zhou L, Lin G, Na Y: Multilocular cystic renal cell carcinoma: an experience of clinical management for 31 cases. J Cancer Res Clin Oncol 2008, 134(4): 433-437.
- Murad T, Komaiko W, Oyasu R, Bauer K: Multilocular cystic renal cell carcinoma. Am J Clin Pathol 1991, 95(5): 633-637.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript