Review Article | Open Access
Research Progress on the Association between Obesity and Prostate Cancer
Hang Xu1, Yingshuang Tang1, Xiaorui Zhang1, Xian Zhang1, Along Kang1
1Department of Pharmacy, 986 Hospital, Fourth Military Medical University, Xi'an, Shaanxi, P.R. China.
Correspondence: Along Kang (Department of Pharmacy, 986 Hospital, Fourth Military Medical University, 269 Youyi East Road, Beilin District, Xi'an 710032, Shaanxi Province, China; Email: kalong1900@163.com.)
Annals of Urologic Oncology 2024, 7(2): 48-54. https://doi.org/10.32948/auo.2024.07.17
Received: 07 Jul 2024 | Accepted: 16 Jul 2024 | Published online: 18 Jul 2024
Key words obesity, prostate cancer, treatment response, prognosis, lifestyle modification, pharmacological treatment, clinical trials, interdisciplinary cooperation, gene-environment interaction, mechanism research
At the same time, the obesity problem is showing an alarming growth trend globally, becoming a public health crisis that cannot be ignored [11-14]. Obesity not only affects an individual's appearance and self-esteem but, more importantly, it is closely related to the development of various chronic diseases, including but not limited to cardiovascular diseases, type 2 diabetes, hypertension, and certain types of cancer [15, 16]. In an obese state, the abnormal accumulation of adipose tissue leads to energy metabolism disorders, chronic low-grade inflammation, insulin resistance, and hormone imbalances [17-20]. These complex physiological and pathological changes collectively increase the risk of various diseases.
Against this backdrop, the complex association between obesity and prostate cancer has gradually attracted widespread attention from researchers [21-24]. Multiple epidemiological studies have shown a significant correlation between obesity and the risk of prostate cancer, disease progression, and prognostication [25-28]. Although the specific mechanisms of this association are not yet fully elucidated, it is attracted significant attention. Understanding the intrinsic links between obesity and prostate cancer not only helps us better understand the pathogenesis of prostate cancer but also provides new ideas and strategies for its prevention, early diagnosis, and personalized treatment [29-31].
Therefore, this review highlights the latest research progress on the association between obesity and prostate cancer. By reviewing relevant literature (provide key words of the study and database surfed), a systematic analysis was performed for potential mechanisms by which obesity affects the occurrence and development of prostate cancer. In this regard, the review provides valuable references for researchers in related fields and raise public awareness of the issue of the association between obesity and prostate cancer. This, in turn, will promote the adoption and dissemination of healthy lifestyles, effectively reducing the incidence and mortality rates of prostate cancer.
Firstly, on a global scale, the incidence of prostate cancer has significantly increased over the past few decades. This trend aligns almost synchronously with the global prevalence of obesity. Obesity, regarded as a "pandemic" of modern society, seems to share a subtle connection with the increasing incidence of prostate cancer [34]. Although it cannot yet be conclusively stated that obesity directly causes prostate cancer, the correlation between the two is undeniable [35, 36]. Further analysis of research results from various geographical regions reveals some inconsistencies regarding the association between obesity and prostate cancer [37, 38]. In developed countries including Europe and North America, where related research began earlier and comprises of comprehensive medical data systems, the research results are relatively rich and in-depth. Some large-scale epidemiological studies indicate that obese men have a significantly higher risk of developing prostate cancer compared to non-obese men [39, 40]. This association is particularly evident in high-grade or advanced prostate cancer. However, in Asian countries such as China, where the incidence of prostate cancer is also on the rise in recent years, studies on the association between obesity and prostate cancer are relatively scarce, and their conclusions are inconsistent [40, 41]. This inconsistency may be related to differences in genetic background, lifestyle, dietary habits, and medical standards across regions. Exploring the association between obesity and prostate cancer, an issue that cannot be ignored is the standardization of obesity definitions. Currently, Body Mass Index (BMI) is widely used as a common indicator for assessing obesity [43]. BMI, is calculated by dividing a person's weight in kilograms by the square of their height in meters, provides a straightforward reflection of an individual's weight status. However, it is important to note that BMI is not a perfect assessment standard, as it does not distinguish between fat and muscle mass, nor does it indicate the distribution of fat within the body. Therefore, relying solely on BMI to evaluate the association between obesity and prostate cancer may have certain limitations. Additionally, the applicability of BMI standards varies among different populations. For instance, Asian populations may have higher body fat percentages and lower muscle mass at the same BMI, suggesting that lower BMI thresholds might be needed to define obesity in these groups [41]. Lastly, it is crucial to emphasize that obesity is not the sole risk factor for prostate cancer. The occurrence of prostate cancer is a complex process involving multiple factors and steps, including interactions among genetic, environmental, and lifestyle factors. Age, family history, dietary habits, and sex hormone levels may all influence the incidence of prostate cancer [44]. Therefore, when discussing the association between obesity and prostate cancer, these factors should be comprehensively considered to avoid viewing obesity as the only or decisive factor. Future research should also explore the interactions between obesity and other risk factors to more comprehensively uncover the pathogenesis of prostate cancer.
Firstly, changes in hormone levels, particularly the imbalance of androgens and insulin-like growth factor (IGF), serve as key links between obesity and the increased risk of prostate cancer [45, 46]. Androgens, as vital hormones in the male body, play a crucial role in the normal growth and development of the prostate [47]. However, when androgen levels are abnormally elevated, they may act as "catalysts" for prostate cancer. In an obese state, adipose tissue is not only an energy reservoir but also an active endocrine organ that secretes various hormones and cytokines, some of which can influence androgen metabolism and function [48]. For example, aromatase in fat cells can convert androgen precursors into estrogens, leading to a relative increase in estrogen levels [47]. Estrogen has been shown to promote the proliferation of prostate cancer cells. Additionally, obesity may indirectly increase the bioavailability of free androgens by affecting the synthesis and secretion of sex hormone-binding globulin (SHBG), thereby further increasing the risk of prostate cancer [48].
Simultaneously, the insulin and insulin-like growth factor (IGF) pathways also play significant roles in the occurrence and development of prostate cancer [49]. Obesity is often associated with insulin resistance and hyperinsulinemia, a condition in which the pancreas secretes more insulin to maintain blood glucose levels. High levels of insulin not only regulate glucose metabolism but also may promote the proliferation and survival of prostate cells by activating pathways such as the IGF-1 receptor (IGF-1R). IGF-1 is a powerful growth factor closely related to the growth, differentiation, and invasiveness of prostate cancer cells. In an obese state, increased secretion of IGF-1 by fat cells, along with enhanced IGF-1 bioactivity due to insulin resistance, acts on prostate tissue and increases the risk of prostate cancer.
Beyond hormonal changes, chronic inflammation is another important factor by which obesity promotes prostate cancer. Chronic low-grade inflammation caused by obesity is an adaptive response to excess fat accumulation. In an obese state, immune cells such as macrophages and T cells in adipose tissue are activated and release a large number of inflammatory factors and chemokines, such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and chemokine CCL7 [50]. These inflammatory mediators not only regulate systemic inflammatory responses but also directly act on prostate tissue, promoting abnormal proliferation and carcinogenesis. CCL7, in particular, is a chemokine secreted by fat cells that can specifically attract prostate tumor cells expressing the CCR3 receptor, creating a microenvironment conducive to tumor growth and metastasis.
Moreover, various bioactive molecules secreted by fat cells influence the occurrence and development of prostate cancer through other pathways. Adipokines such as leptin, adiponectin, and resistin play crucial roles in regulating energy metabolism, immune responses, and cell proliferation [51]. Leptin, for example, is considered a potential pro-carcinogenic factor that can promote the proliferation and invasion of prostate tumor cells by activating multiple signaling pathways [52]. In contrast, adiponectin has anti-tumor effects, and its levels decrease in obesity, potentially weakening the body's defense against prostate cancer [53].
Finally, obesity may indirectly promote the occurrence and development of prostate cancer by affecting immune responses and increasing oxidative stress. In an obese state, the immune system may undergo functional changes, such as reduced immune cell numbers and decreased functionality, which can impair the body's ability to surveil and eliminate prostate cancer cells. Additionally, obesity is accompanied by increased oxidative stress, with excessive free radicals and oxidative products potentially damaging prostate cell DNA, increasing the risk of genetic mutations and carcinogenesis. These mechanisms collectively make obesity a significant risk factor for the occurrence and development of prostate cancer.
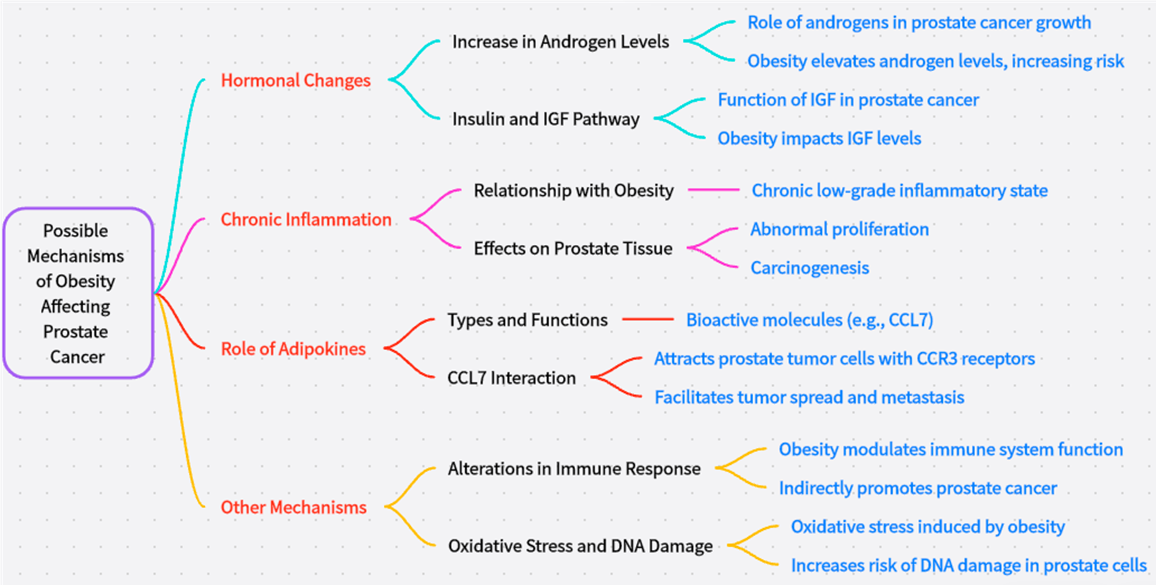 Figure 1. Possible mechanisms of obesity affecting prostate cancer.
Figure 1. Possible mechanisms of obesity affecting prostate cancer.Firstly, obese patients may experience various weight-related adverse reactions during prostate cancer treatment. Drug therapy, a crucial component of comprehensive prostate cancer treatment, often sees its efficacy influenced by the patient's weight and drug metabolism capacity. Due to the higher fat content in obese patients, drug distribution and metabolism in the body can change, affecting the bioavailability and therapeutic effect of medications. For example, certain chemotherapeutic drugs may have a reduced clearance rate in obese patients, leading to higher drug concentrations and an increased risk of toxic side effects. Additionally, obesity can affect the response to hormone therapy, as hormonal imbalances in obese individuals may interfere with the effectiveness of such treatments.
Surgical treatment is another key modality for prostate cancer, but obese patients face higher risks during surgery [56, 57]. Increased abdominal fat in obese patients complicates the surgical field, making the procedure more challenging and increasing the difficulty of surgical maneuvers. This not only prolongs the surgery time but also raises the incidence of surgical complications such as bleeding, infection, and wound healing. Moreover, obesity can affect patients' responses to anesthesia, heightening the risk of postoperative respiratory and cardiovascular complications.
Beyond adverse reactions during treatment, obesity significantly increases the risk of disease progression and recurrence in prostate cancer patients. The persistent presence of chronic inflammation and abnormal secretion of adipokines in obese individuals create a favorable environment for the growth and spread of prostate cancer cells. These inflammatory factors and adipokines not only promote the proliferation and invasiveness of prostate cancer cells but also may alter the immune status of the tumor microenvironment, making it easier for tumor cells to evade immune surveillance and elimination. Consequently, obese patients often have higher recurrence rates and faster disease progression after treatment compared to non-obese patients.
Ultimately, obesity also significantly affects the overall mortality and prostate cancer-specific mortality rates in these patients. Numerous studies have shown that obesity is a critical predictor of poor prognosis in prostate cancer patients [58]. Due to the combined effects of metabolic disorders, reduced immune function, and lower treatment tolerance, obese patients have significantly higher all-cause and prostate cancer-specific mortality rates than non-obese patients. This not only increases the risk of patient death but also adds to the burden on healthcare resources and socioeconomic costs.
In summary, obesity plays a crucial role in the treatment and prognosis of prostate cancer. To improve treatment outcomes and prognosis for obese prostate cancer patients, a multifaceted approach is necessary. This includes optimizing treatment plans, enhancing perioperative management, controlling body weight, and promoting healthier lifestyles. Additionally, further research into the mechanisms linking obesity and prostate cancer is needed to provide a scientific basis for developing more precise and effective treatment strategies.
Firstly, lifestyle modifications are fundamental and critical in preventing prostate cancer, particularly for obese patients [60, 61]. This requires individuals to fundamentally change unhealthy habits and adopt a healthier lifestyle. Maintaining a balanced diet means reducing the intake of high-fat, high-calorie foods and increasing the proportion of vegetables, fruits, whole grains, and high-quality protein-rich foods to ensure adequate nutrition without overburdening the body. Additionally, regular physical activity is indispensable. It promotes metabolism, enhances cardiovascular function, and helps maintain a healthy weight. For those who are already overweight or obese, gradual weight loss through a reasonable diet and regular exercise can positively impact reducing the risk of prostate cancer.
Besides lifestyle changes, pharmacological treatments offer new possibilities for intervening in mechanisms related to obesity and prostate cancer [62, 63]. With advances in medical research, scientists are gradually uncovering the complex interactions between obesity and prostate cancer, leading to the development of various potential therapeutic drugs. For example, targeted drugs against the chemokine receptor CCR3 have shown promising prospects in prostate cancer treatment. These drugs specifically block the binding of the CCR3 receptor to its ligands, interfering with the migration and invasion processes of prostate cancer cells and thus inhibiting tumor progression. Although these drugs are currently in clinical trials, their unique mechanisms and preliminary efficacy data have garnered widespread attention. As research progresses and technology advances, these drugs are expected to offer more personalized and precise treatment options for prostate cancer patients.
Lastly, regular check-ups and screenings are invaluable for the early detection of prostate cancer, significantly improving treatment outcomes and survival rates [65, 66]. This is particularly important for high-risk groups, such as obese individuals. Regular prostate cancer screenings, including serum prostate-specific antigen (PSA) testing and digital rectal exams, can detect potential prostate cancer lesions early, allowing timely intervention. Additionally, for patients already diagnosed with prostate cancer, regular follow-ups and check-ups are essential. They enable doctors to monitor disease progression and treatment response, adjusting treatment plans to achieve optimal results.
In summary, clinical interventions and preventive measures play a vital role in mitigating the impact of obesity on prostate cancer. Through proactive lifestyle adjustments, rational use of pharmacological treatments, and strengthened regular check-ups and screenings, we can effectively reduce the risk of prostate cancer, improve treatment outcomes, and enhance the quality of life for patients (Figure 2).
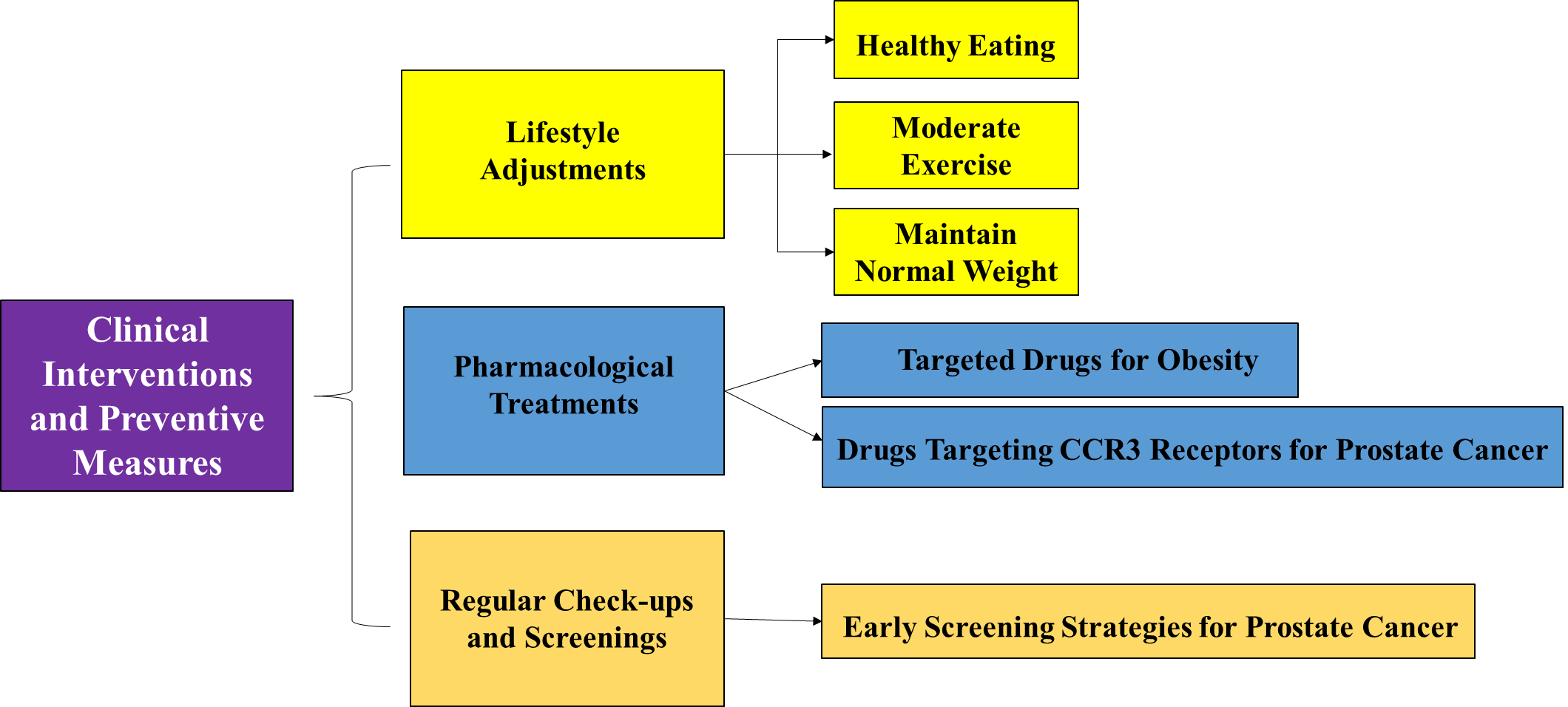 Figure 2. Clinical interventions and preventive measures.
Figure 2. Clinical interventions and preventive measures.
Furthermore, the design of clinical trials is a crucial direction for future research. To more accurately assess the impact of obesity on prostate cancer and the efficacy of various interventions, there is need to design more scientific and comprehensive clinical trials. These trials should fully consider individual patient differences, the diversity of treatment regimens, and the necessity of long-term follow-up to ensure the reliability and reproducibility of results. Additionally, with the advent of the precision medicine era, one should explore clinical trial designs based on personalized information such as patient genotype and metabolic state to provide more precise treatment recommendations.
Interdisciplinary collaboration plays a vital role in addressing the association between obesity and prostate cancer. Close cooperation among disciplines such as endocrinology, oncology, and nutrition will provide broader perspectives and richer resources, promoting rapid development in this field. By combining research findings and technological methods from various disciplines, we can gain a deeper understanding of the interaction mechanisms between obesity and prostate cancer. This approach can lead to the development of more effective prevention and treatment strategies.This interdisciplinary collaboration not only enhances the breadth and depth of research but also facilitates the translation and application of research outcomes, contributing to patient health and well-being.
In conclusion, the complex association between obesity and prostate cancer and its potential mechanisms still require continuous exploration and in-depth research. Through the implementation of comprehensive intervention measures, including healthy lifestyle adjustments, appropriate pharmacological treatments, and regular check-ups and screenings, can effectively reduce the risk of prostate cancer and improve patient prognosis. Looking to the future, the call for more interdisciplinary cooperation and communication to jointly advance the development of this field and contribute wisdom and strength to overcoming this challenge.
None.
Ethical policy
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Approval from institutional ethical committee was taken.
Availability of data and materials
All data generated or analysed during this study are included in this publication.
Author contributions
Hang Xu, Yingshuang Tang searched academic literature and wrote the draft manuscript; Xiaorui Zhang and Xian Zhang did the data analysis and language editing; Along Kang supervised the review writting progress and approved the final manuscript submission.
Competing interests
Authors report no conflict of interest.
Funding
None.
- Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE: The 2016 WHO classification of tumours of the urinary system and male genital organs—part B: prostate and bladder tumours. Eur Urol 2016, 70(1): 106-119.
- Merriel SWD, Funston G, Hamilton W: Prostate cancer in primary care. Adv Ther 2018, 35(9): 1285-1294.
- Scher HI, Leibel S, Fuks Z: Cancer of the prostate. In: DeVita, Hellman, and Rosenberg's Cancer Principles and Practices of Oncology 2015: 932-980.
- Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA: Prostate cancer in young men: an important clinical entity. Nat Rev Urol 2014, 11(6): 317-323.
- Young RH: Tumors of the prostate gland, seminal vesicles, male urethra, and penis. Am J Surg Pathol 2000.
- Holst J: Global Health - emergence, hegemonic trends and biomedical reductionism. Glob Health 2020, 16(1): 42.
- Adisa TA, Gbadamosi G, Adekoya OD: Gender apartheid: The challenges of breaking into "man's world." Gend Work Organ 2021, 28(6): 2216-2234.
- Wang L, Lu B, He M, Wang Y, Wang Z, Du L: Prostate cancer incidence and mortality: global status and temporal trends in 89 countries from 2000 to 2019. Front Public Health 2022, 10: 811044.
- Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A: Recent global patterns in prostate cancer incidence and mortality rates. Eur Urol 2020, 77(1): 38-52.
- Van Poppel H, Albreht T, Basu P, Hogenhout R, Collen S, Roobol M: Serum PSA-based early detection of prostate cancer in Europe and globally: past, present and future. Nat Rev Urol 2022, 19(9): 562-572.
- Mohajan D, Mohajan HK: Obesity and its related diseases: a new escalating alarming in global health. J Innov Med Res 2023, 2(3): 12-23.
- Azeez TA: Obesity in Africa: The challenges of a rising epidemic in the midst of dwindling resources. Obes Med 2022, 31: 100397.
- Pallangyo P, Mkojera ZS, Hemed NR, Swai HJ, Misidai N, Mgopa L, Bhalia S, Millinga J, Mushi TL, Kabeya L, et al: Obesity epidemic in urban Tanzania: a public health calamity in an already overwhelmed and fragmented health system. BMC Endocr Disord 2020, 20(1): 1-9.
- Lobstein T, Cooper K: Obesity: A ghost at the feast of the sustainable development goals. Curr Obes Rep 2020, 9(4): 470-478.
- Robinson E, Haynes A, Sutin A, Daly M: Self-perception of overweight and obesity: a review of mental and physical health outcomes. Obes Sci Pract 2020, 6(5): 552-561.
- Gow ML, Tee MSY, Garnett SP, Baur LA, Aldwell K, Thomas S, Lister NB, Paxton SJ, Jebeile H: Physical activity based pediatric obesity treatment, depression, self-esteem and body image: A systematic review with meta-analysis. Ment Health Phys Act 2020, 19: 100342.
- Kawai T, Autieri MV, Scalia R: Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol 2021, 320(3): C375-C391.
- Kojta I, Chacińska M, Błachnio-Zabielska A: Obesity, bioactive lipids, and adipose tissue inflammation in insulin resistance. Nutrients 2020, 12(5): 1305.
- Zatterale F, Longo M, Naderi J, Raciti GA, Desiderio A, Miele C, Beguinot F: Chronic adipose tissue inflammation linking obesity to insulin resistance and type 2 diabetes. Front Physiol 2020, 10: 1607.
- Lu Z, Li Y, Song J: Characterization and treatment of inflammation and insulin resistance in obese adipose tissue. Diabetes Metab Syndr Obes 2020: 3449-3460.
- Santos-Pereira M, Pereira SC, Rebelo I, Spadella MA, Oliveira PF, Alves MG: Decoding the influence of obesity on prostate cancer and its transgenerational impact. Nutrients 2023, 15(23): 4858.
- Lan N, Lu Y, Zhang Y, Pu S, Xi H, Nie X, Liu J, Yuan W: FTO—a common genetic basis for obesity and cancer. Front Genet 2020, 11: 559138.
- Zhu Y, Mo M, Wei Y, Wu J, Pan J, Freedland SJ, Zheng Y, Ye D: Epidemiology and genomics of prostate cancer in Asian men. Nat Rev Urol 2021, 18(5): 282-301.
- Kim DS, Scherer PE: Obesity, diabetes, and increased cancer progression. Diabetes Metab J 2021, 45(6): 799-812.
- Wilson RL, Taaffe DR, Newton RU, Hart NH, Lyons-Wall P, Galvão DA: Obesity and prostate cancer: A narrative review. Crit Rev Oncol Hematol 2022, 169: 103543.
- Zhu D, Toker M, Shyr W, Fram E, Watts KL, Agalliu I: Association of obesity and diabetes with prostate cancer risk groups in a multiethnic population. Clin Genitourin Cancer 2022, 20(3): 299-299.e10.
- Kensler KH, Rebbeck TR: Cancer progress and priorities: prostate cancer. Cancer Epidemiol Biomarkers Prev 2020, 29(2): 267-277.
- Adesunloye BA: Mechanistic insights into the link between obesity and prostate cancer. Int J Mol Sci 2021, 22(8): 3935.
- Baio R, Napodano G, Caruana C, Molisso G, Di Mauro U, Intilla O, Pane U, D'Angelo C, Francavilla AB, Guarnaccia C, et al: Association between obesity and frequency of high-grade prostate cancer on biopsy in men: A single center retrospective study. Mol Clin Oncol 2022, 17(2): 1-11.
- Rivera-Izquierdo M, Pérez de Rojas J, Martínez-Ruiz V, Arrabal-Polo MÁ, Pérez-Gómez B, Jiménez-Moleón JJ: Obesity and biochemical recurrence in clinically localized prostate cancer: a systematic review and meta-analysis of 86,490 patients. Prostate Cancer Prostatic Dis 2022, 25(3): 411-421.
- Saha A, Kolonin MG, DiGiovanni J: Obesity and prostate cancer—microenvironmental roles of adipose tissue. Nat Rev Urol 2023, 20(10): 579-596.
- Role of Herbal Medicines: Management of Lifestyle Diseases. Springer Nature, 2023.
- Gao H, Zhao Y, Zhao L, Wang Z, Yan K, Gao B, Zhang L: The role of oxidative stress in multiple exercise-regulated bone homeostasis. Aging Dis 2023, 14(5): 1555.
- Boubertakh B, Silvestri C, Di Marzo V: Obesity: The fat tissue disease version of cancer. Cells 2022, 11(12): 1872.
- Grigore AD: Reassessment of neurite-like processes in a neuroendocrine prostate cancer model. Rice University, 2020.
- Kodada D, Hyblova M, Krumpolec P, Janostiakova N, Barath P, Grendar M, Blandova G, Petrovic O, Janega P, Repiska V, et al: The potential of liquid biopsy in detection of endometrial cancer biomarkers: a pilot study. Int J Mol Sci 2023, 24(9): 7811.
- Daniels JP, Freedland SJ, Gresham G: The growing implications of obesity for prostate cancer risk and mortality: where do we go from here? JNCI J Natl Cancer Inst 2023, 115(12): 1448-1450.
- Salibi G: Obesity and prostate cancer: the influence of metabolic syndromes. Spec J Med Acad Other Life Sci 2023, 1(2).
- Papavasileiou G, Tsilingiris D, Spyrou N, Vallianou NG, Karampela I, Magkos F, Dalamaga M: Obesity and main urologic cancers: current systematic evidence, novel biological mechanisms, perspectives and challenges. Semin Cancer Biol 2023, 91: 70-98.
- Fernandez CJ, George AS, Subrahmanyan NA, Pappachan JM: Epidemiological link between obesity, type 2 diabetes mellitus and cancer. World J Methodol 2021, 11(3): 23-45.
- Zhu Y, Mo M, Wei Y, Wu J, Pan J, Freedland SJ, Zheng Y, Ye D: Epidemiology and genomics of prostate cancer in Asian men. Nat Rev Urol 2021, 18(5): 282-301.
- Qiang JK, Lipscombe LL, Lega IC: Association between diabetes, obesity, aging, and cancer: review of recent literature. Transl Cancer Res 2020, 9(9): 5743.
- Mohajan D, Mohajan HK: Body mass index (BMI) is a popular anthropometric tool to measure obesity among adults. J Innov Med Res 2023, 2(4): 25-33.
- Haffner MC, Zwart W, Roudier MP, True LD, Nelson WG, Epstein JI, De Marzo AM, Nelson PS, Yegnasubramanian S: Genomic and phenotypic heterogeneity in prostate cancer. Nat Rev Urol 2021, 18(2): 79-92.
- Zhao C, Hu W, Xu Y, Wang D, Wang Y, Lv W, Xiong M, Yi Y, Wang H, Zhang Q, et al: Current landscape: the mechanism and therapeutic impact of obesity for breast cancer. Front Oncol 2021, 11: 704893.
- Pagano C, di Zazzo E, Avilia G, Savarese B, Navarra G, Proto MC, Fiore D, Rienzo M, Gazzerro P, Laezza C, et al: Advances in “adiponcosis”: insights in the inner mechanisms at the base of adipose and tumour tissues interplay. Int J Cancer 2023, 152(12): 2464-2473.
- Hou Z, Huang S, Li Z: Androgens in prostate cancer: a tale that never ends. Cancer Lett 2021, 516: 1-12.
- J Felgueiras, V Camilo, M Fardilha, C Jerónimo: More than androgens: hormonal and paracrine signaling in prostate development and homeostasis. Tissue-Specif Cell Signal 2020: 195-223.
- Holly JMP, Biernacka K, Perks CM: The role of insulin-like growth factors in the development of prostate cancer. Expert Rev Endocrinol Metab 2020, 15(4): 237-250.
- López-Ortega O, Moreno-Corona NC, Cruz-Holguin VJ, Garcia-Gonzalez LD, Helguera-Repetto AC, Romero-Valdovinos M, Arevalo-Romero H, Cedillo-Barron L, León-Juárez M: The immune response in adipocytes and their susceptibility to infection: a possible relationship with infectobesity. Int J Mol Sci 2022, 23(11): 6154.
- Umar MI, Hassan W, Murtaza G, Buabeid M, Arafa E, Irfan HM, Asmawi MZ, Huang X: The adipokine component in the molecular regulation of cancer cell survival, proliferation and metastasis. Pathol Oncol Res 2021, 27: 1609828.
- Borowski A, Siemińska L: Serum omentin levels in patients with prostate cancer and associations with sex steroids and metabolic syndrome. J Clin Med 2020, 9(4): 1179.
- Nigro E, Daniele A, Salzillo A, Ragone A, Naviglio S, Sapio L: AdipoRon and other adiponectin receptor agonists as potential candidates in cancer treatments. Int J Mol Sci 2021, 22(11): 5569.
- Castagneto-Gissey L, Casella-Mariolo J, Casella G, Mingrone G: Obesity surgery and cancer: what are the unanswered questions? Front Endocrinol 2020, 11: 213.
- Santos-Pereira M, Pereira SC, Rebelo I, Spadella MA, Oliveira PF, Alves MG: Decoding the influence of obesity on prostate cancer and its transgenerational impact. Nutrients 2023, 15(23): 4858.
- Gillessen S, Attard G, Beer TM, Beltran H, Bjartell A, Bossi A, Briganti A, Bristow RG, Chi KN, Clarke N, et al: Management of patients with advanced prostate cancer: report of the advanced prostate cancer consensus conference 2019. Eur Urol 2020, 77(4): 508-547.
- Ghiassi S, El Chaar M, Aleassa EM, Moustarah F, El Djouzi S, Birriel TJ, Rogers AM: ASMBS position statement on the relationship between obesity and cancer, and the role of bariatric surgery: risk, timing of treatment, effects on disease biology, and qualification for surgery. Surg Obes Relat Dis 2020, 16(6): 713-724.
- Zhu D, Toker M, Shyr W, Fram E, Watts KL, Agalliu I: Association of obesity and diabetes with prostate cancer risk groups in a multiethnic population. Clin Genitourin Cancer 2022, 20(3): 299-299.e10.
- Takura T, Hirano Goto K, Honda A: Development of a predictive model for integrated medical and long-term care resource consumption based on health behaviour: application of healthcare big data of patients with circulatory diseases. BMC Med 2021, 19(1): 1-16.
- Yannitsos D, Murphy RA, Pollock P, Di Sebastiano KM: Facilitators and barriers to participation in lifestyle modification for men with prostate cancer: a systematic review. Eur J Cancer Care 2020, 29(1): e13193.
- Gandaglia G, Leni R, Bray F, Fleshner N, Freedland SJ, Kibel A, Stattin P, Van Poppel H, La Vecchia C: Epidemiology and prevention of prostate cancer. Eur Urol Oncol 2021, 4(6): 877-892.
- Rubinstein MM, Brown KA, Iyengar NM: Targeting obesity-related dysfunction in hormonally driven cancers. Br J Cancer 2021, 125(4): 495-509.
- Saha A, Kolonin MG, DiGiovanni J: Obesity and prostate cancer—microenvironmental roles of adipose tissue. Nat Rev Urol 2023, 20(10): 579-596.
- Gómez Rivas J, Leenen RCA, Venderbos LDF, Helleman J, de la Parra I, Vasilyeva V, Moreno-Sierra J, Basu P, Chandran A, van den Bergh RCN, et al: Navigating through the controversies and emerging paradigms in early detection of prostate cancer: bridging the gap from classic RCTs to modern population-based pilot programs. J Pers Med 2023, 13(12): 1677.
- Hansen MF: Clinical characteristics, survival rate and patients’ perceptions among patients diagnosed with prostate cancer receiving treatment at Ocean Road Cancer Institute in Dar Es Salaam, Tanzania: a mixed-method study. 2022.
- Hussain SH, Huertas CS, Mitchell A, Deman AL, Laurenceau E: Biosensors for circulating tumor cells (CTCs)-biomarker detection in lung and prostate cancer: trends and prospects. Biosens Bioelectron 2022, 197: 113770.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript