Case Report | Open Access
Incidental Detection of Papillary Renal Cell Carcinoma in Nephrectomy Specimen for Chronic Pyelonephritis
Sana Ahuja1, Adil Aziz Khan1, Sufian Zaheer11Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
Correspondence: Sufian Zaheer (Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India; Email: sufianzaheer@gmail.com).
Annals of Urologic Oncology 2024, 7(2): 75-78. https://doi.org/10.32948/auo.2024.06.01
Received: 29 May 2024 | Accepted: 07 Jun 2024 | Published online: 08 Jun 2024
Abstract
Papillary renal cell carcinoma (PRCC), though often asymptomatic in its early stages, presents unique diagnostic challenges. This case report describes the serendipitous discovery of a 1cm PRCC nodule initially missed on radiological investigations. Through meticulous pathological evaluation, PRCC was identified, underscoring the crucial interplay between urological and pathological perspectives. Therapeutic decisions, guided by tumor characteristics and clinical considerations, highlighted the necessity for comprehensive multidisciplinary collaboration. This case emphasizes the importance of thorough evaluation and interdisciplinary cooperation in optimizing diagnostic accuracy and therapeutic strategies in renal pathology.
Key words papillary renal cell carcinoma, nephrectomy specimen, chronic pyelonephritis, incidental
Key words papillary renal cell carcinoma, nephrectomy specimen, chronic pyelonephritis, incidental
Introduction
The incidental discovery of papillary renal cell carcinoma (PRCC) within nephrectomy specimens excised for chronic pyelonephritis presents a unique clinical scenario, often compounded by the challenges of radiological oversight. Uncommonly encountered, especially when initial radiological investigations fail to detect subtle lesions, this phenomenon underscores the intricacies of renal pathology and the importance of comprehensive evaluation [1-2].
While PRCC constitutes a significant subset of renal cell carcinomas, its detection within the context of chronic pyelonephritis adds complexity to diagnostic and therapeutic decision-making. Radiological imaging, while invaluable in renal pathology assessment, may overlook small lesions amidst the backdrop of chronic inflammatory changes, as evidenced in this case. The failure to identify a 1cm PRCC nodule on initial radiological investigations highlights the rarity and diagnostic intricacies associated with such occurrences.
In this report, we delineate a comprehensive case of incidental PRCC detection within a nephrectomy specimen excised for chronic pyelonephritis, emphasizing the uncommon nature of such findings and the pivotal role of meticulous pathological evaluation in uncovering diagnostic nuances. This case underscores the necessity for heightened awareness among clinicians, radiologists, and pathologists regarding the potential coexistence of renal malignancies in the setting of chronic inflammatory conditions, thereby guiding optimal patient management.
While PRCC constitutes a significant subset of renal cell carcinomas, its detection within the context of chronic pyelonephritis adds complexity to diagnostic and therapeutic decision-making. Radiological imaging, while invaluable in renal pathology assessment, may overlook small lesions amidst the backdrop of chronic inflammatory changes, as evidenced in this case. The failure to identify a 1cm PRCC nodule on initial radiological investigations highlights the rarity and diagnostic intricacies associated with such occurrences.
In this report, we delineate a comprehensive case of incidental PRCC detection within a nephrectomy specimen excised for chronic pyelonephritis, emphasizing the uncommon nature of such findings and the pivotal role of meticulous pathological evaluation in uncovering diagnostic nuances. This case underscores the necessity for heightened awareness among clinicians, radiologists, and pathologists regarding the potential coexistence of renal malignancies in the setting of chronic inflammatory conditions, thereby guiding optimal patient management.
Case presentation
A 31-year-old male presented with recurrent urinary tract infections and left flank pain refractory to conservative management. The pain was dull aching, moderate to severe in intensity and non-radiating in nature. There was no history of hematuria, pyuria, or bilateral lower limb edema. There was history of right percutaneous nephrostomy placement because of right non-functioning kidney secondary to right pelvic-ureteric junction obstruction one month back. Contrast-enhanced computed tomography urography was done and revealed focal xanthogranulomatous pyelonephritis with moderate hydronephrosis in the right kidney with evidence of luminal narrowing and wall thickening in the right upper ureter extending into the pelvi-ureteric junction (Figure 1a, b). The patient was further evaluated with a 99mTc-DTPA (Diethylene triamine penta acetate radioisotope renogram which revealed a non-functioning right kidney. Thus, a simple nephrectomy was advised. Intraoperatively, there were dense peri-ureteric and peripelvic adhesions present. The excised specimen was excised and sent for histopathological examination.
Cut surface of the kidney exhibited loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter. Also seen was a small 1 cm solid grey white nodule near the upper pole of the right kidney (Figure 1c). Hematoxylin and eosin-stained sections showed dilated calyces, tubular atrophy and thyroidization. Also seen were dense lymphomononuclear interstitial infiltrate and glomerulosclerosis with periglomerular fibrosis. However, the nodule which was observed on microscopy exhibited an invasive tumor arranged as papillae. These papillae were lined by cuboidal to columnar cells with eosinophilic cytoplasm with inconspicuous nucleoli (ISUP grade 1). Few sheets of foamy histiocytes were also seen in between the papillae. On IHC, the tumor cells were positive for CK7 and focally for CD10 (Figure 2). Thus, a final diagnosis of an incidentally detected papillary renal carcinoma (pT1) in a background of chronic pyelonephritis was made. The postoperative recovery was uneventful.
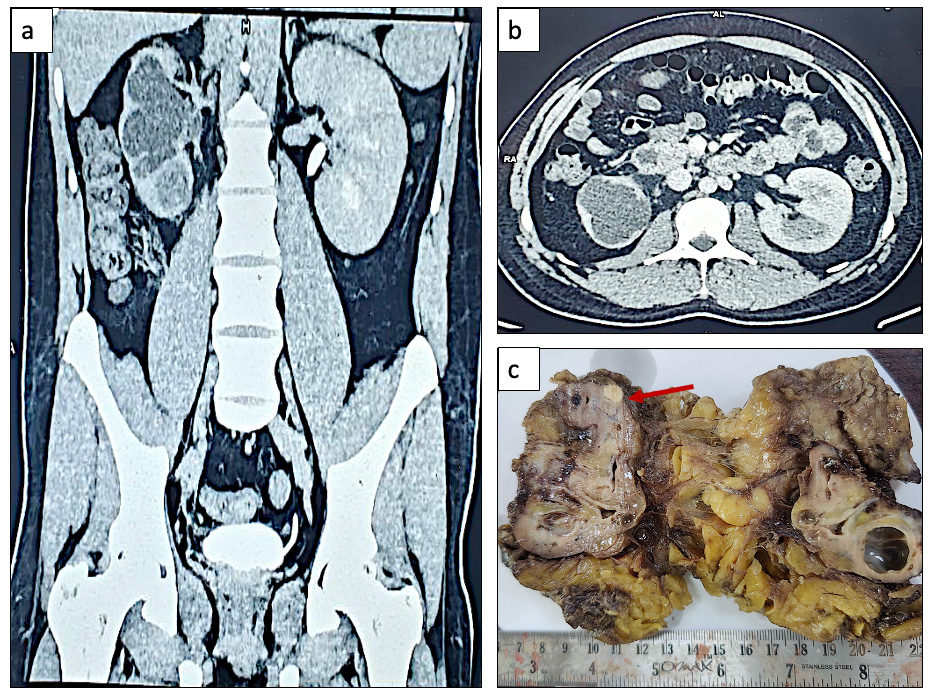 Figure 1. Radiological and gross images. (a, b) Contrast-enhanced computed tomography urography revealed moderate hydronephrosis in the right kidney with evidence of luminal narrowing and wall thickening in the right upper ureter. (c) Gross examination revealed loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter; A small 1 cm solid grey white nodule was observed near the upper pole of the right kidney (marked with red arrow).
Figure 1. Radiological and gross images. (a, b) Contrast-enhanced computed tomography urography revealed moderate hydronephrosis in the right kidney with evidence of luminal narrowing and wall thickening in the right upper ureter. (c) Gross examination revealed loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter; A small 1 cm solid grey white nodule was observed near the upper pole of the right kidney (marked with red arrow).
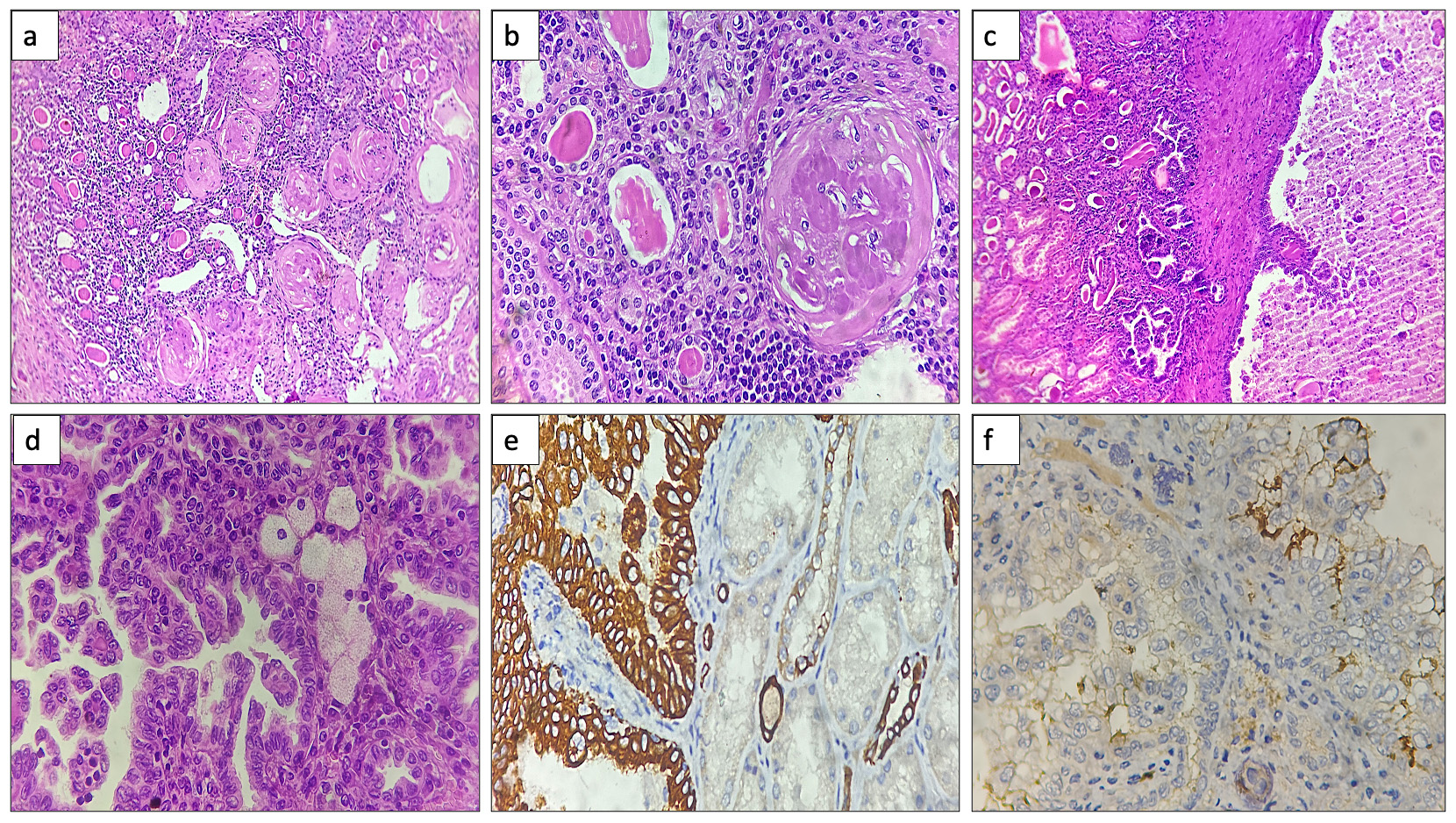 Figure 2. Histopathological photomicrographs. (a, b) Hematoxylin and eosin stained sections exhibited tubular atrophy, thyroidization, glomerulosclerosis and dense lymphomononuclear interstitial infiltrate (10x, 40x). (c) Sections examined show the interface of the papillary renal cell carcinoma with the surrounding kidney (10x). (d) Hematoxylin and eosin-stained sections exhibited papillae lined by columnar cells along with presence of foamy histiocytes (40x). (e, f) Immunohistochemistry exhibited positive immunostaining for CK7 and CD10 (focal) (40x).
Figure 2. Histopathological photomicrographs. (a, b) Hematoxylin and eosin stained sections exhibited tubular atrophy, thyroidization, glomerulosclerosis and dense lymphomononuclear interstitial infiltrate (10x, 40x). (c) Sections examined show the interface of the papillary renal cell carcinoma with the surrounding kidney (10x). (d) Hematoxylin and eosin-stained sections exhibited papillae lined by columnar cells along with presence of foamy histiocytes (40x). (e, f) Immunohistochemistry exhibited positive immunostaining for CK7 and CD10 (focal) (40x).
Cut surface of the kidney exhibited loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter. Also seen was a small 1 cm solid grey white nodule near the upper pole of the right kidney (Figure 1c). Hematoxylin and eosin-stained sections showed dilated calyces, tubular atrophy and thyroidization. Also seen were dense lymphomononuclear interstitial infiltrate and glomerulosclerosis with periglomerular fibrosis. However, the nodule which was observed on microscopy exhibited an invasive tumor arranged as papillae. These papillae were lined by cuboidal to columnar cells with eosinophilic cytoplasm with inconspicuous nucleoli (ISUP grade 1). Few sheets of foamy histiocytes were also seen in between the papillae. On IHC, the tumor cells were positive for CK7 and focally for CD10 (Figure 2). Thus, a final diagnosis of an incidentally detected papillary renal carcinoma (pT1) in a background of chronic pyelonephritis was made. The postoperative recovery was uneventful.
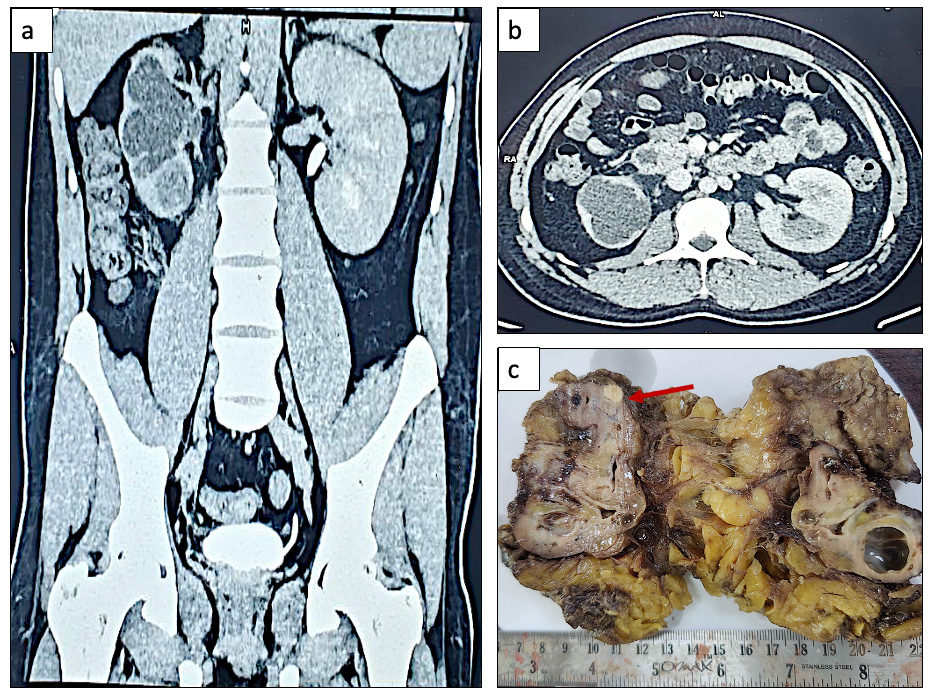 Figure 1. Radiological and gross images. (a, b) Contrast-enhanced computed tomography urography revealed moderate hydronephrosis in the right kidney with evidence of luminal narrowing and wall thickening in the right upper ureter. (c) Gross examination revealed loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter; A small 1 cm solid grey white nodule was observed near the upper pole of the right kidney (marked with red arrow).
Figure 1. Radiological and gross images. (a, b) Contrast-enhanced computed tomography urography revealed moderate hydronephrosis in the right kidney with evidence of luminal narrowing and wall thickening in the right upper ureter. (c) Gross examination revealed loss of corticomedullary differentiation with few dilated cysts ranging in size from 2 cm to 4 cm in diameter; A small 1 cm solid grey white nodule was observed near the upper pole of the right kidney (marked with red arrow).
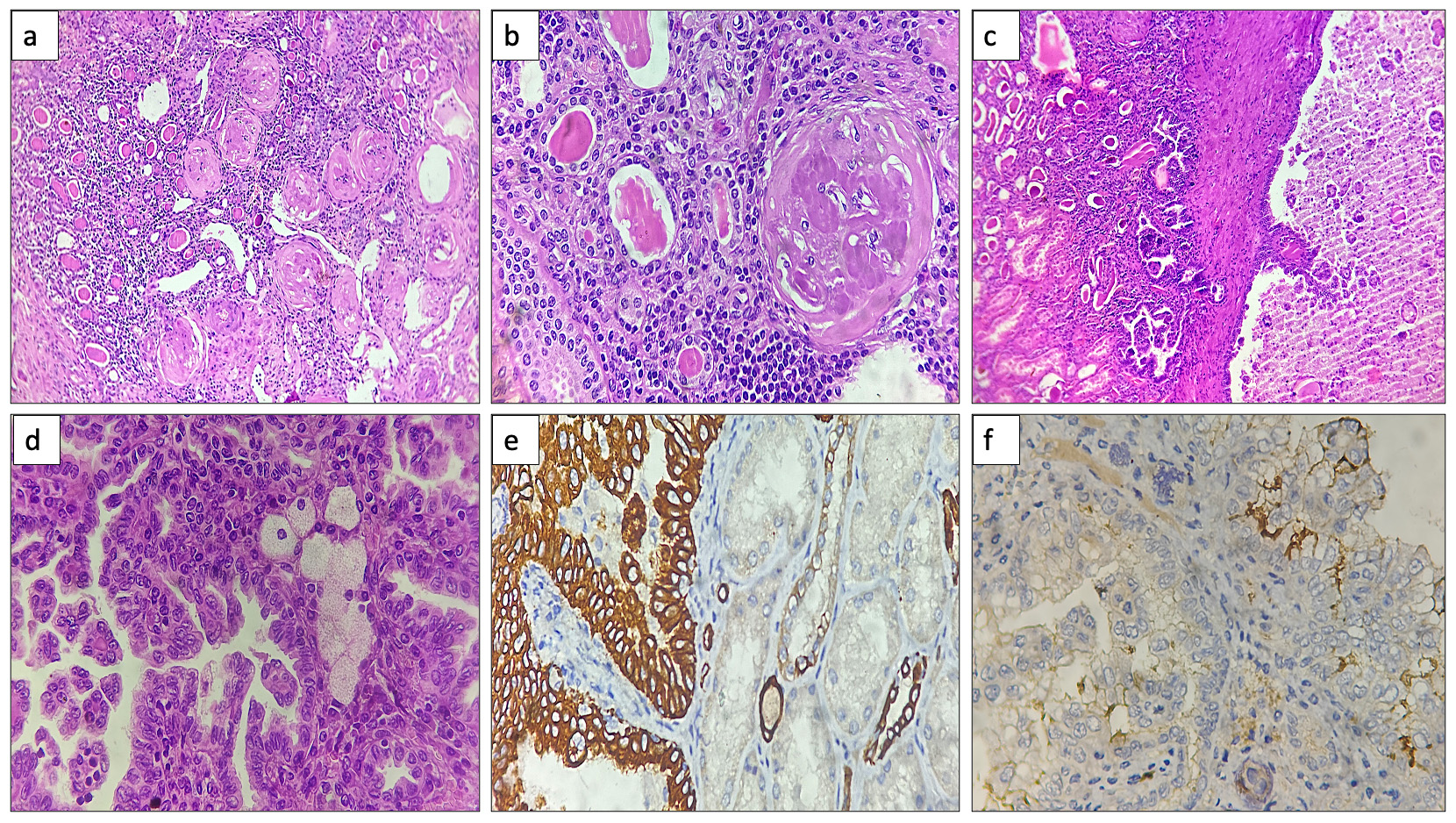 Figure 2. Histopathological photomicrographs. (a, b) Hematoxylin and eosin stained sections exhibited tubular atrophy, thyroidization, glomerulosclerosis and dense lymphomononuclear interstitial infiltrate (10x, 40x). (c) Sections examined show the interface of the papillary renal cell carcinoma with the surrounding kidney (10x). (d) Hematoxylin and eosin-stained sections exhibited papillae lined by columnar cells along with presence of foamy histiocytes (40x). (e, f) Immunohistochemistry exhibited positive immunostaining for CK7 and CD10 (focal) (40x).
Figure 2. Histopathological photomicrographs. (a, b) Hematoxylin and eosin stained sections exhibited tubular atrophy, thyroidization, glomerulosclerosis and dense lymphomononuclear interstitial infiltrate (10x, 40x). (c) Sections examined show the interface of the papillary renal cell carcinoma with the surrounding kidney (10x). (d) Hematoxylin and eosin-stained sections exhibited papillae lined by columnar cells along with presence of foamy histiocytes (40x). (e, f) Immunohistochemistry exhibited positive immunostaining for CK7 and CD10 (focal) (40x).
Discussion
Papillary renal cell carcinoma (PRCC) is characterized by papillary architecture and typically presents as a solid enhancing mass on imaging [3]. Radiological imaging, including computed tomography (CT) and magnetic resonance imaging (MRI), serves as the cornerstone for initial assessment in suspected renal pathologies. However, small lesions, particularly those measuring 1cm or less, can evade detection, especially amidst the backdrop of chronic pyelonephritis-associated changes. In our case, the 1cm PRCC nodule was initially missed on radiological investigations, emphasizing the limitations of imaging modalities in detecting subtle lesions in the presence of confounding inflammatory changes.
The definitive diagnosis of PRCC often relies on histopathological examination of tissue specimens obtained through biopsy or surgical resection. In our case, meticulous examination of the nephrectomy specimen revealed characteristic features of PRCC, including papillary architecture and clear cell cytoplasm. Pathological evaluation not only confirmed the presence of PRCC but also provided crucial insights into tumor characteristics such as grade, extent of invasion, and margin status, guiding further management decisions.
The management of incidentally discovered PRCC within the context of chronic pyelonephritis necessitates careful consideration of various factors, including tumor size, location, histological subtype, and patient comorbidities [3]. The incidental detection of PRCC within a nephrectomy specimen underscores the importance of comprehensive evaluation and interdisciplinary collaboration in renal pathology. This case highlights the need for heightened awareness among radiologists and urologists regarding the potential coexistence of renal malignancies in the setting of chronic inflammatory conditions. Additionally, it emphasizes the critical role of pathologists in the meticulous examination of surgical specimens to uncover incidental findings and provide accurate diagnoses, thereby guiding optimal patient management.
Few cases of renal cell carcinoma arising in end-stage renal disease have been reported in excised non-functioning kidneys. Coban et al in their study on 163 patients with non-functioning kidneys who underwent nephrectomy reported 4 (2.5%) cases of incidentally detected renal cell carcinoma [1]. Semjén et al reported that among 2566 nephrectomies excised for RCC, 31 developed in a background of end-stage renal disease out of which there were 5 papillary renal cell carcinomas [2]. Guguloth et al described a rare case of Grade 3 papillary renal carcinoma masquerading as pyelonephritis in a 62 year old male [4].
The case of incidental PRCC detection within a nephrectomy specimen for chronic pyelonephritis underscores the intricate interplay between radiological, pathological, and clinical aspects of renal pathology. Addressing the challenges posed by radiological limitations, optimizing pathological evaluation, and carefully considering therapeutic implications are essential for ensuring timely diagnosis and appropriate management. In poorly functioning or non-functioning kidneys, renal tumors may be missed on radiological examination. Therefore a meticulous gross and microscopic examination is crucial.
The definitive diagnosis of PRCC often relies on histopathological examination of tissue specimens obtained through biopsy or surgical resection. In our case, meticulous examination of the nephrectomy specimen revealed characteristic features of PRCC, including papillary architecture and clear cell cytoplasm. Pathological evaluation not only confirmed the presence of PRCC but also provided crucial insights into tumor characteristics such as grade, extent of invasion, and margin status, guiding further management decisions.
The management of incidentally discovered PRCC within the context of chronic pyelonephritis necessitates careful consideration of various factors, including tumor size, location, histological subtype, and patient comorbidities [3]. The incidental detection of PRCC within a nephrectomy specimen underscores the importance of comprehensive evaluation and interdisciplinary collaboration in renal pathology. This case highlights the need for heightened awareness among radiologists and urologists regarding the potential coexistence of renal malignancies in the setting of chronic inflammatory conditions. Additionally, it emphasizes the critical role of pathologists in the meticulous examination of surgical specimens to uncover incidental findings and provide accurate diagnoses, thereby guiding optimal patient management.
Few cases of renal cell carcinoma arising in end-stage renal disease have been reported in excised non-functioning kidneys. Coban et al in their study on 163 patients with non-functioning kidneys who underwent nephrectomy reported 4 (2.5%) cases of incidentally detected renal cell carcinoma [1]. Semjén et al reported that among 2566 nephrectomies excised for RCC, 31 developed in a background of end-stage renal disease out of which there were 5 papillary renal cell carcinomas [2]. Guguloth et al described a rare case of Grade 3 papillary renal carcinoma masquerading as pyelonephritis in a 62 year old male [4].
The case of incidental PRCC detection within a nephrectomy specimen for chronic pyelonephritis underscores the intricate interplay between radiological, pathological, and clinical aspects of renal pathology. Addressing the challenges posed by radiological limitations, optimizing pathological evaluation, and carefully considering therapeutic implications are essential for ensuring timely diagnosis and appropriate management. In poorly functioning or non-functioning kidneys, renal tumors may be missed on radiological examination. Therefore a meticulous gross and microscopic examination is crucial.
Declaration
Acknowledgements
Not applicable.
Ethical policy
The study was done in accordance with the Declaration of Helsinki. Informed patient consent was taken.
Availability of data and materials
That data is available from the corresponding author on request.
Author contributions
Sana Ahuja: conceptualisation, data curation, formal analysis, writing original draft; Adil Aziz: conceptualisation, formal analysis, review and writing; Sufian Zaheer: conceptualisation, resources, data curation, supervision, review and editing.
Competing interests
The authors have no conflicts of interest to declare.
Funding
None.
Not applicable.
Ethical policy
The study was done in accordance with the Declaration of Helsinki. Informed patient consent was taken.
Availability of data and materials
That data is available from the corresponding author on request.
Author contributions
Sana Ahuja: conceptualisation, data curation, formal analysis, writing original draft; Adil Aziz: conceptualisation, formal analysis, review and writing; Sufian Zaheer: conceptualisation, resources, data curation, supervision, review and editing.
Competing interests
The authors have no conflicts of interest to declare.
Funding
None.
References
- Coban G, Tekden BC, Şahin N, Toluk Ö, Toprak H, Yıldız P, İlktaç A: Unexpected Discoveries: Uncovering Incidental Tumors in Simple Nephrectomy Specimens. Revista Médica Clínica Las Condes 2023, 34(6): 421-426.
- Semjén D, Dénes B, Somorácz Á, Fintha A, Forika G, Jenei A, Dobi D, Micsik T, Eizler KV, Giba N, et al: Renal Cell Carcinoma in End-Stage Renal Disease: A Retrospective Study in Patients from Hungary. Pathobiology 2023, 90(5): 322-332.
- Angori S, Lobo J, Moch H: Papillary renal cell carcinoma: current and controversial issues. Curr Opin Urol 2022, 32(4): 344-351.
- Guguloth MN, Manzoor J, Kuchana SK, Suvvari TK, Gopu AR, Kunden VD, Bhattarai S, Anand A: Sporadic unilateral papillary renal cell carcinoma masquerading pyelonephritis: A case report. Clin Case Rep 2023, 11(2): e6976.
Cite this article: Ahuja S, Khan AA, Zaheer S: Incidental Detection of Papillary Renal Cell Carcinoma in Nephrectomy Specimen for Chronic Pyelonephritis. Ann Urol Oncol 2024, 7(2): 75-78. https://doi.org/10.32948/auo.2024.06.01
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript