Case Report | Open Access
Unveiling the Rarity: A Case Report on Gigantic Primary Scrotal Lipoma
Sumanta Das1, Adil Aziz Khan21Department of Pathology, Fortis Memorial Research Institute, Gurugram, India.
2Department of Pathology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
Annals of Urologic Oncology 2024, 7(2): 70-74. https://doi.org/10.32948/auo.2024.06.30
Received: 08 May 2024 | Accepted: 30 Jun 2024 | Published online: 01 Jul 2024
Key words scrotal lipoma, testicular malignancy, lnguinal-scrotal hernia
Hydroceles, collections of fluid within the tunica vaginalis surrounding the testis, present as painless scrotal swelling and are usually benign but can occasionally be associated with underlying testicular pathology [5]. Inguinal-scrotal hernia, which occurs when abdominal contents protrude through the inguinal canal into the scrotum, presents as a soft, reducible mass that may increase in size with activities like coughing or straining [6]. Epididymal cysts, benign fluid-filled sacs arising from the epididymis, are generally asymptomatic and discovered incidentally during physical examination or imaging studies [7].
An exceptionally rare differential diagnosis is primary scrotal lipoma, which poses a unique diagnostic challenge. Primary scrotal lipomas arise from the subcutaneous fat of the scrotal sac, and clinical examinations often struggle to differentiate them from testicular or para-testicular swellings [8]. We present a case of a primary gigantic scrotal lipoma in an adult male, confirmed through histopathological examination. The patient, a 45-year-old man, reported a progressively enlarging scrotal mass over several years. He denied any pain, urinary symptoms, or systemic manifestations. On physical examination, a large, non-tender, and mobile mass was palpated in the scrotum, distinct from the testes. Initial differential diagnoses included hydrocele, inguinal-scrotal hernia, and a para-testicular tumor.
Ultrasonography was employed as the first-line imaging modality, revealing a well-circumscribed, hyperechoic mass separate from the testes, suggestive of a lipomatous lesion. Given the uncertainty of the diagnosis, surgical exploration was undertaken. Intraoperatively, a large, encapsulated fatty mass was identified, arising from the scrotal subcutaneous tissue and completely separate from the testicular and spermatic structures. The excised mass was subjected to histopathological examination, confirming the diagnosis of a lipoma. The histological analysis demonstrated mature adipose tissue without any evidence of malignancy. This case underscores the importance of considering primary scrotal lipoma in the differential diagnosis of scrotal swellings and the role of histopathological confirmation in establishing the diagnosis [9].
Primary scrotal lipomas are exceptionally rare benign tumors that originate from the subcutaneous fat of the scrotal sac. Due to their rarity and non-specific presentation, they often pose a diagnostic challenge. Clinically, primary scrotal lipomas can be indistinguishable from other scrotal masses, as physical examination alone is often insufficient to delineate their exact nature and origin [10]. They typically present as slow-growing, painless masses that can attain considerable size before diagnosis. The etiology of scrotal lipomas remains unclear, though some hypotheses suggest a possible embryological origin or association with chronic irritation or trauma [9].
The clinical diagnosis of primary scrotal lipoma is challenging due to its rarity and non-specific presentation. Ultrasonography can aid in differentiating lipomas from other scrotal masses, but definitive diagnosis often requires histopathological confirmation. Fine-needle aspiration cytology (FNAC) and magnetic resonance imaging (MRI) may also be useful adjuncts in ambiguous cases [1]. Surgical excision is the treatment of choice for primary scrotal lipomas, providing both diagnostic confirmation and symptomatic relief. The prognosis is excellent, as these tumors are benign with no known potential for malignant transformation. Recurrence is rare following complete surgical removal [11].
Scrotal swellings encompass a wide range of differential diagnoses, each necessitating careful clinical and diagnostic evaluation. Primary scrotal lipoma, although rare, should be considered in the differential diagnosis, especially in cases where typical features of more common conditions are absent. This case highlights the importance of considering rare entities in differential diagnoses and the role of histopathology in confirming the diagnosis of primary scrotal lipoma. Future studies and case reports will be invaluable in enhancing our understanding and management of this uncommon condition.
On clinical examination, a well-defined, non-reducible, non-tender mass approximately 15 cm in size was palpated in the right scrotal region. The right testis was not palpable due to the enormous size of the mass. Given the substantial swelling, a scrotal ultrasonography was performed, which revealed a hyperechoic homogeneous solid mass with weak vascularization, measuring 17.2 x 12 x 6 cm. The mass was compressing the right testis (Figure 1). Based on these findings, a neoplastic etiology was suspected, and surgical excision was planned.
An inguinoscrotal incision was made during the surgery, revealing an intact right testis and epididymis. A giant encapsulated tumor, slightly adhered to the tunica vaginalis, was identified and meticulously removed. The tumor was sent for histopathological examination. Grossly, the tumor appeared to be lipomatous in origin, and on serial sectioning, no necrosis or variegated areas were observed (Figure 1).
Histopathological examination confirmed the diagnosis of a primary scrotal lipoma. The analysis revealed mature adipocytes arranged in lobules, separated by fibrovascular septa (Figure 2). No atypical cells, anaplasia, or other heterologous components were noted in various sections of the tumor tissue. The adjacent testis appeared normal, with no evidence of any testicular lesion.
The diagnosis of primary scrotal lipoma was established based on these histopathological features. The patient was followed up for the next six months post-operatively, during which no recurrence of the lipoma was observed. The patient reported significant relief from discomfort and a return to normal daily activities following the surgery.
This case underscores the importance of considering primary scrotal lipoma in the differential diagnosis of scrotal swellings, especially in instances where the presentation does not align with more common conditions such as hydrocele, varicocele, or testicular tumors. The gradual growth of the mass without pain can lead to delayed medical consultation, as seen in this case. Timely imaging and histopathological evaluation are crucial for accurate diagnosis and appropriate management. Surgical excision not only provides definitive diagnosis but also symptomatic relief and prevention of potential complications arising from large scrotal masses.
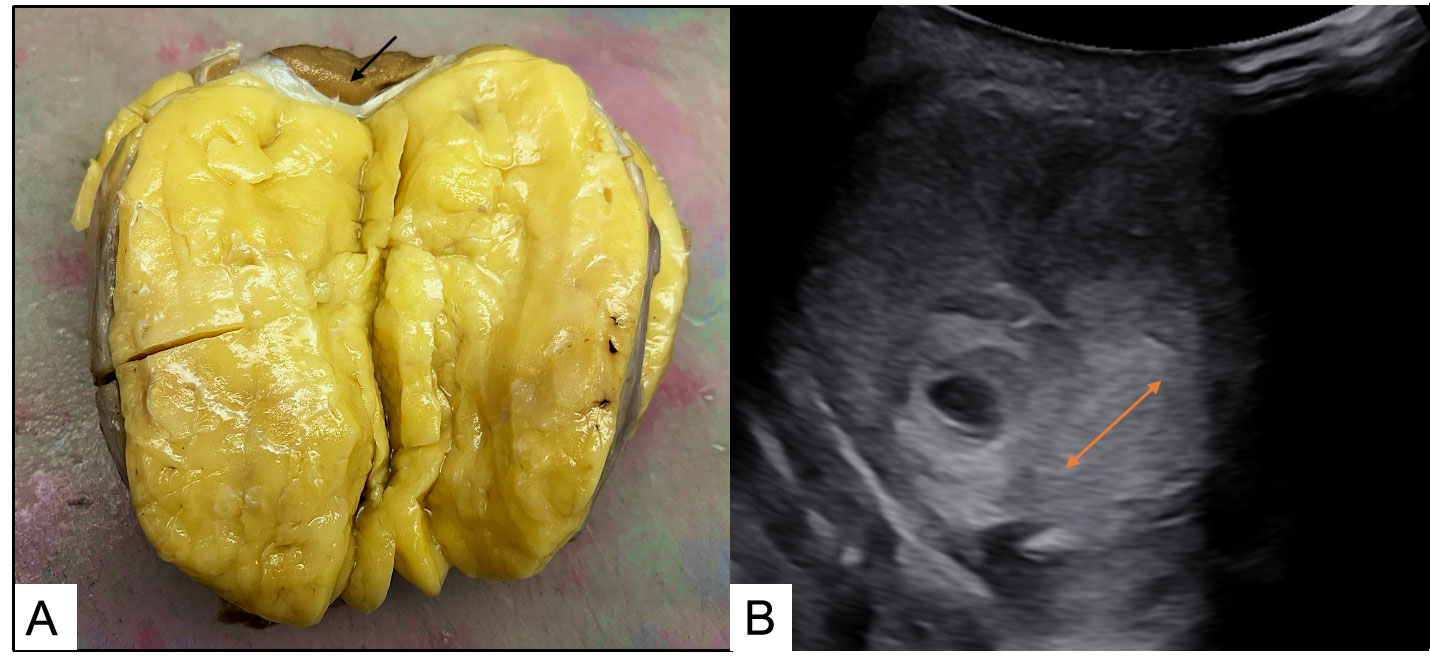 Figure 1: A) Gross image showing an encapsulated lipomatous lesion with normal compressed testes in periphery marked by arrow; B) Ultrasonographic picture showing weakly vascularized homogenous mass in right scrotum marked by arrow.
Figure 1: A) Gross image showing an encapsulated lipomatous lesion with normal compressed testes in periphery marked by arrow; B) Ultrasonographic picture showing weakly vascularized homogenous mass in right scrotum marked by arrow.
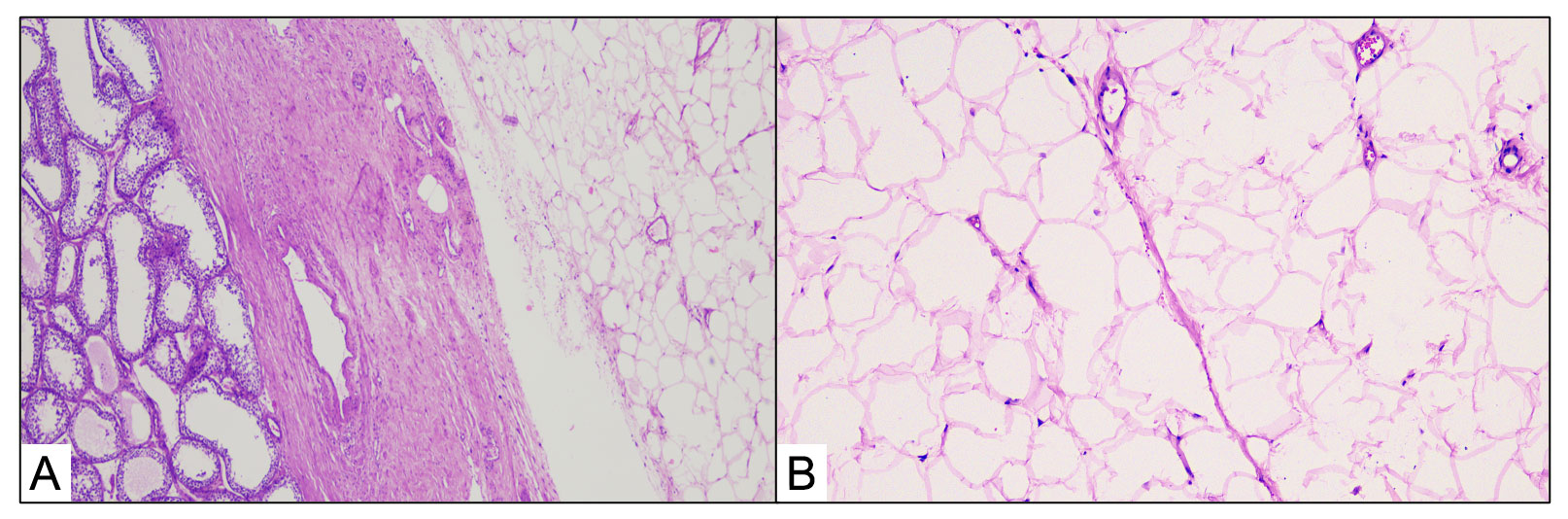 Figure 2: A) Histological image showing lipoma and adjacent normal testes (H & E 100X); B) Histological picture showing mature adipose tissue with no atypical cells (H & E 400X).
Figure 2: A) Histological image showing lipoma and adjacent normal testes (H & E 100X); B) Histological picture showing mature adipose tissue with no atypical cells (H & E 400X).
Typically, the first symptom of a scrotal lipoma is a sensation of fullness in the scrotum, which later progresses to an evident swelling. Radiological investigations, particularly ultrasonography, play a crucial role in diagnosing scrotal lipomas. Ultrasonography usually reveals a homogenous and hyperechoic mass, which helps differentiate it from other types of scrotal masses. However, in cases involving a large mass, distinguishing a benign lipoma from a malignancy can be challenging.
One important differential diagnosis to consider is well-differentiated liposarcoma, which accounts for 3% to 7% of extratesticular tumors. Key histopathological features of a lipoma include mature adipose tissue without atypical cells or heterologous elements. Magnetic resonance imaging (MRI) is thought to be a useful modality for differentiating between well-differentiated liposarcoma and lipoma. Jasper et al. [12] reported a case of primary scrotal lipoma in a 40-year-old male which was initially diagnosed as hydrocele. Another similar case was reported by Ibrahim et al. [10] in a young male whose size was approximately similar to the present case. The comparison of previous reported cases is shown in Table 1.
The only effective management for scrotal lipomas is surgical resection, primarily because a neoplastic entity needs to be ruled out definitively. In the present case, a giant mass was identified and excised, which was subsequently confirmed to be a lipoma through histopathological examination. This finding is extremely rare, underscoring the importance of including lipoma in the differential diagnosis when encountering non-reducible and painless scrotal swellings.
Surgical excision not only provides definitive diagnosis but also symptomatic relief and prevents potential complications arising from large scrotal masses. Moreover, timely intervention can alleviate the psychological distress associated with the fear of malignancy. Postoperative follow-up is crucial to monitor for any signs of recurrence, although recurrence is rare following complete surgical removal.
In conclusion, while primary scrotal lipomas are rare, they should be considered in the differential diagnosis of scrotal swellings, especially in cases where the presentation does not align with more common conditions such as hydrocele, varicocele, or testicular tumors. This case highlights the clinical presentation, diagnostic approach, and successful management of a primary giant scrotal lipoma, emphasizing the necessity of considering rare entities in clinical practice to ensure comprehensive patient care. Further research and case reports will be invaluable in enhancing our understanding and management of this uncommon condition.
|
Table 1. Comparison of previous reported cases. |
||||||
|
Author |
Age |
Radiological Finding |
Size (cm) |
Initial Diagnosis |
Imaging Modality |
Histopathological Findings |
|
Zarami, et al. [10] |
42 |
Not available |
60 |
Not available |
Not available |
Mature adipocytes, no atypia, encapsulated mass |
|
Mbwambo, et al. [12] |
40 |
Vascularized and heterogeneous lesion |
10 |
Not available |
Not available |
Mature adipocytes, no atypia |
|
Forsmann, et al. [13] |
75 |
Not available |
10 & 10.3 |
Inguinal hernia |
Not available |
Mature adipocytes, fat necrosis |
|
Ibrahim, et al. [14] |
23 |
Hyperechoic homogenous solid mass |
12.7 |
Not available |
Ultrasound, MRI |
Mature adipocytes, no atypia |
|
Louis, et al. [15] |
46 |
Heterogenous solid mass with weak vascularization |
16 |
Hydrocele |
Ultrasonography, MRI |
Well-differentiated and mature adipocytes |
|
Present Case |
37 |
Hyperechoic homogenous solid mass with weak vascularization |
17.2 |
Testicular tumor |
Ultrasound |
Mature adipocytes, no atypia, encapsulated mass |
Not Applicable.
Ethical policy
The study was done in accordance with the Declaration of Helsinki. Informed patient consent was taken.
Availability of data and materials
That data is available from the corresponding author on request.
Author contributions
Adil Aziz Khan: writing original draft, editing; Sumanta Das: formal analysis, data curation, conceptualization, supervision.
Competing interests
The authors have no conflicts of interest to declare.
Funding
None.
- Barbosa JABA, Arap MA: Acute scrotum: differential diagnosis and treatment. Revista de Medicina 2018, 97(3): 278-282.
- Ghuman NK, Singh P, Raikar S: Male infertility-evaluation and management at a glance. Fertil Sci Res 2020, 7(1): 26-36.
- Kravvas G, Ge L, Ng J, Shim T, Doiron P, Watchorn R, Kentley J, Panou E, Dinneen M, Freeman A: The management of penile intraepithelial neoplasia (PeIN): clinical and histological features and treatment of 345 patients and a review of the literature. J Dermatol Treat 2022, 33(2): 1047-1062.
- Jensen CFS, Østergren P, Dupree JM, Ohl DA, Sønksen J, Fode M: Varicocele and male infertility. Nat Rev Urol 2017, 14(9): 523-533.
- Dagur G, Gandhi J, Suh Y, Weissbart S, Sheynkin YR, Smith NL, Joshi G, Khan SA: Classifying hydroceles of the pelvis and groin: an overview of etiology, secondary complications, evaluation, and management. Curr Urol 2017, 10(1): 1-14.
- Tran HM, MacQueen I, Chen D, Simons M: Systematic review and guidelines for management of scrotal inguinal hernias. J Abdom Wall Surg 2023, 2: 11195.
- Boscarelli A, Bellini T: Epididymal cyst in children. Euro J Pediatrics 2021, 180: 2723-2729.
- Novara G, Iafrate M, Ficarra V: Painless Scrotal Lumps: Classification and Clinics. Scrotal Pathol 2012Epub ahead of print.: 139-149.
- Berevoescu N-I, Stanilescu S, Halcu G, Berevoescu M, Cristian D: Large primary scrotal lipoma with particular presentation. Int Surg J 2019, 6(2): 597-600.
- Zarami AB, Ibrahim H, Ibrahim A: Giant scrotal lipoma: case report and review of the literature. J Case Rep Images Urol 2018, 3: 100009Z100015AZ102019.
- Srivastava K, Agarwal A, Vikram SSS, Gupta M: Huge scrotal lipoma posing a diagnostic dilemma: a case report and review of literature. Urol Case Rep 2017, 15: 39-41.
- Mbwambo OJ, Pallangyo A, Mbwambo JS, Bright F, Mteta AK, Bogdanowicz J, Ngowi BN: Primary scrotal lipoma posing a diagnostic quandary: Experience from northern Tanzania, a case report. Clin Case Rep 2023, 11(6): e7503.
- Forsmann M, McLaughlin D, Leonard T: A case report of scrotal lipoma and review of lipoma pathogenesis. J Surg Case Rep 2022, 2022(5): rjac214.
- Ballout I, Awad R, Al Ali B, Chamma L, Issa H, Moussa M: Huge primary scrotal lipoma: Case report and review of literature. Urol Case Rep 2023, 51: 102586.
- Vignot L, Saad E, Peyromaure M, Barry Delongchamps N: Giant Primary Scrotal Lipoma: A Rare Entity with Diagnostic Pitfalls. Case Rep Urol 2020, 2020:8815845.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript