Review Article | Open Access
Diagnosis and Treatment of Adrenal Metastasis in Modern Era
Sarah E. Matusofsky1, *, Paris M. Fang1, *, Ellie R. Monnette1, Austin M. Kim2, Mark R. Wakefield1, 3
1Department of Surgery, University of Missouri School of Medicine, Columbia, MO, USA.
2Department of Microbiology, Immunology & Pathology, Des Moines University, Des Moines, IA, USA.
3Ellis Fischel Cancer Center, University of Missouri School of Medicine, Columbia, MO, USA.
*These authors contribute equally.
Correspondence: Mark R. Wakefield (Department of Surgery, University of Missouri School of Medicine, Columbia, MO, 65212, USA; Email: wakefieldmr@health.missouri.edu).
Annals of Urologic Oncology 2023, 6(4): 127-131. https://doi.org/10.32948/auo.2023.11.07
Received: 27 Oct 2023 | Accepted: 09 Nov 2023 | Published online: 11 Nov 2023
Key words adrenal metastatic tumors, biopsy, imaging
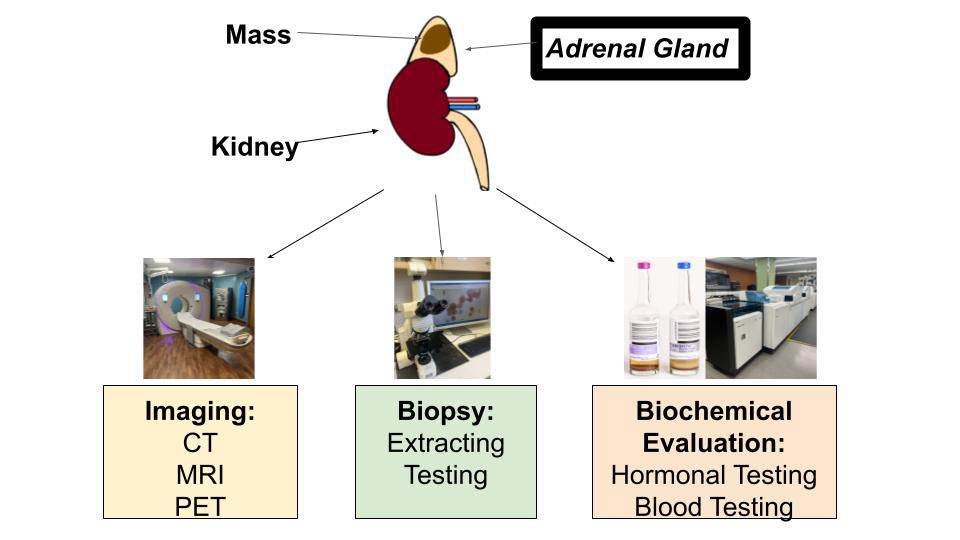 Figure 1. Methods for Evaluation of Adrenal Metastasis. Imaging techniques (left), biopsy (middle) and biochemical evaluation (right) are important methods used for detection of adrenal metastasis.
Figure 1. Methods for Evaluation of Adrenal Metastasis. Imaging techniques (left), biopsy (middle) and biochemical evaluation (right) are important methods used for detection of adrenal metastasis.
Imaging
The management of the primary malignancy is influenced by the presence of metastases. Although most adrenal tumors belong to the category of benign, many of these tumors are indeterminate on imaging with current technology. Computed tomography (CT), ultrasound scan (US), and the combination of CT and US are the most commonly used types of scans used for adrenal biopsies [18]. Based on current studies, there is not a single scan with 100% dependability that can comprehensively evaluate adrenal incidentalomas or a scan with close to 100% dependability for distinguishing malignant from benign adrenal masses. In addition, many of these scans have limitations. For example, ultrasounds can be limited in larger patients [18]. CT and magnetic resonance imaging (MRI) scans are often used to identify benign lesions and are not used for adrenal malignancy. These scans depict lipid content, which shows whether an adrenal mass is benign (high lipid content) or potentially malignant (low lipid content). However, with CT, 30% of adrenal lesions have been incorrectly classified [19]. Fluorodeoxyglucose- positron emission tomography, or FDG-PET, and CT scans are mainly only used to detect the presence of malignant diseases. Previous imaging can be used for comparison, which can help determine the timeline of the metastasis and change over time. Further evaluation is recommended for patients with cancer that appears to have metastasized to only the adrenal glands and no other sites in the body. The choice of screening modality depends on many factors, including metastasis progression, prognosis, resources available and physician preference.
(1) CT: The adrenal mass CT protocol includes a pre-contrast scan, a portal venous phase scan, and a delay scan [20]. On CT, adrenal metastases are typically heterogeneous and have an unenhanced density greater than 10 HU. Only assessing precontrast density by itself is not specific enough because one-third of benign adrenal masses have an HU greater than 10 and have low lipid content, which are the main indicators of potentially malignant masses. In these cases, a CT scan with contrast enhancement for washout characteristics is necessary. An adrenal lesion with a precontrast HU of less than 10 is unlikely to be malignant, but in patients with extra-adrenal malignancy, there is a pooled false negative rate of 7%. In these cases, special attention should be paid to adrenal masses with even precontrast HUs of less than 10. In order to achieve better accuracy, the measurement of HU should be standardized. In measurement, two-thirds of the largest axial diameter of the region of interest should be included. Boundaries should be avoided whenever possible. If areas of necrosis are present, the measurement is inaccurate. Because large adrenal masses often include areas of necrosis, calcification, and hemorrhage, neither CT scans or MRIs are able to define their nature [19]. Adrenal masses that are greater than four centimeters are more likely to be malignant. Rapidly growing adrenal lesions, local invasion, irregular borders, and central necrosis are all good indicators of the presence of primary adrenal malignancy and adrenal metastasis. Although often found in large adrenal masses, calcification is seldom seen in metastases of the adrenal glands.
(2) MRI: MRI plays a very small role in characterizing lipid-poor masses. It plays an even smaller role in identifying adrenal masses based on pre-contrast HU values, especially values greater than 20-30 HU, which is very evident in adrenal metastases. The specific MRI that is used regularly is the chemical shift imaging technique [21]. This phenomenon conveys the differential precession frequencies of protons in lipids in water using the same imaging voxel. Many of the adrenal gland carcinomas are visual with high signal intensity on in-phase imaging and low signal intensity on out-of-phase imaging, allowing a simple visual test to be completed by the chemical shift technique. The most efficient and effective way to analyze a lesion in the adrenal gland is using the splenic intensity offered from the CSI technique [22]. However, MRI requires a lot of equipment and needles that are MRI compatible, which are typically costly [18].
(3) PET: An 18F-fluorodeoxyglucose PET (18F-FDG PET) cannot precisely mark cancer cells. However, PET is very useful when determining whether an adrenal mass is benign or malignant and the primary cancer is known because PET has high sensitivity (74-100%) and high specificity (66-100%). PET-CT cannot adequately distinguish adrenal metastases from adrenocortical carcinoma and is subject to both false-positive and false-negative results. PET-MRI offers a higher accuracy compared to PET-CT in diagnoses of other metastases, including liver metastases [23].
Biochemical evaluation
Differentiating pheochromocytoma from metastases cannot be confidently done with CT, MRI, or PET scans, so it is crucial to rule out pheochromocytoma in patients with extra-adrenal malignancy with an indeterminate mass. Plasma fractionated metanephrines elevated over 4x the normal amount or elevated 24-h urinary fractionated metanephrines are important in diagnosing pheochromocytoma [24]. Patients with Cushing syndrome and primary hyperaldosteronism-or other hyperfunctioning-would benefit from additional individualized hormone work up. Hormonal workup is unlikely to have much benefit for patients with poor prognosis. It is recommended for all patients with suspected adrenal metastases on both glands to be clinically evaluated for adrenal insufficiency as, in some cases, it has been linked to adrenal insufficiency. Adrenal insufficiency is not typical when only one adrenal gland is affected, so evaluation for insufficiency is usually not needed. There is a chance of glucocorticoid-related adrenal suppression occurring in patients who have a history of cancer and take glucocorticoids. Procedures should be taken to prevent adrenal crisis.
Biopsy
Patients with a high likelihood of having a malignant mass are often referred for biopsy when imaging techniques (CT, MRI, PET) are insufficient in determining whether an adrenal mass is benign or malignant [25]. It is important to note that needle biopsy may not yield satisfactory results in every patient [26]. FNA, an abbreviation for CT-guided fine-needle aspiration, is practical when trying to confirm the presence of metastatic disease in adrenal lesions as it has a positive predictive value of 100%. FNA is especially useful if the management of the cancer patient would be altered with information from histology. In images with masses that have not been conclusively identified as benign and adrenal masses that are hormonally inactive, FNA is a useful method for determination. However, FNA can also yield non-diagnostic results (0-28% of the time). Complications arise 2.5%-13% of the time and can include adrenal hemorrhage, pain, pancreatitis, and hematuria. Because of the possible risk of hypertensive crisis and other life-threatening complications that could arise in the patient, it is crucial that pheochromocytoma is not included in any biochemical testing that is conducted before the biopsy. FNA should be ruled out if the adrenal lesion is likely to be adrenocortical carcinoma because of the high risk of dissemination which makes it R0 resection impractical. R0 resection refers to a surgical procedure aimed at achieving complete removal of the tumor along with clear margins.
In lung cancer patients with solitary adrenal masses, surgical resection improves prognosis for the primary cancer. It is recommended that the primary cancer be resected or able to be cured by chemotherapy before further consideration of laparoscopic adrenalectomy because of the likelihood of tumor regrowth if the primary cancer is not resected [5]. Uniquely, the standard approach in treating adrenal malignancies with origins from renal cancers is selective inclusion of ipsilateral adrenalectomy with radical nephrectomy rather than routine or considered adrenalectomy [27]. However, adrenal malignancies from renal cancers are often as a result of local invasion of renal cancer cells to the ipsilateral adrenal gland rather than traditional metastasis of the renal cancer [28].
None.
Ethical policy
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Approval from institutional ethical committee was taken.
Availability of data and materials
All data generated or analysed during this study are included in this publication.
Author contributions
Mark R. Wakefield initiated the idea and supervised the whole process. Sarah E. Matusofsky and Paris M. Fang wrote the draft. Ellie R. Monnette drafted Figure 1. Austin M. Kim, Mark R. Wakefield made the critical revision to the draft.
Competing interests
The authors report no conflict of interest.
Funding
None.
- Cingam SR, Mukkamalla SKR, Karanchi H: Adrenal Metastasis. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing 2023 Jan.
- Vincent JM, Morrison ID, Armstrong P, Reznek, RH: The size of normal adrenal glands on computed tomography. Clin Radiol 1994, 49(7): 453-455.
- Shiue K, Song A, Teh BS, Ellis RJ, Yao M, Mayr NA, Huang Z, Sohn J, Machtay M, Lo SS: Stereotactic body radiation therapy for metastasis to the adrenal glands. Expert Rev Anticancer Ther 2012, 12(12): 1613-1620.
- Shaheen O, Ghibour A, Alsaid B: Esophageal Cancer Metastases to Unexpected Sites: A Systematic Review. Gastroenterol Res Pract 2017, 2017: 1657310.
- Kawai N, Tozawa K, Yasui T, Moritoki Y, Sasaki H, Yano M, Fujii Y, Kohri K: Laparoscopic adrenalectomy for solitary adrenal metastasis from lung cancer. JSLRS 2014, 18(3): e2014.00062.
- Almeida MQ, Bezerra-Neto JE, Mendonça BB, Latronico AC, Fragoso MCBV: Primary malignant tumors of the adrenal glands. Clinics 2018, 73(suppl 1): e756s.
- Klikovits T, Lohinai Z, Fábián K, Gyulai M, Szilasi M, Varga J, Baranya E, Pipek O, Csabai I, Szállási Z: New insights into the impact of primary lung adenocarcinoma location on metastatic sites and sequence: A multicenter cohort study. Lung Cancer 2018, 126: 139-148.
- Blažeković I, Jukić T, Granić R, Punda M, Franceschi M: An Unusual Case of Papillary Thyroid Carcinoma Iodine-131 Avid Metastasis to the Adrenal Gland. Acta Clinica Croatica 2018, 57(2): 372-376.
- Teegen EM, Mogl MT, Pratschke J, Rayes N: Adrenal Metastasis of Hepatocellular Carcinoma in Patients following Liver Resection or Liver Transplantation: Experience from a Tertiary Referral Center. Int J Surg Oncol 2018, 2018: 4195076.
- Haider AA, Ruiz de Villa A, Frimer L, Bazikian Y: Metastasis of Melanoma to the Adrenal Glands: A Case Report and Literature Review. Cureus 2022, 14(7): e26749.
- Crimì F, Quaia E, Cabrelle G, Zanon C, Pepe A, Regazzo D, Tizianel I, Scaroni C, Ceccato F: Diagnostic Accuracy of CT Texture Analysis in Adrenal Masses: A Systematic Review. Int J Mol Sci 2022, 23(2): 637.
- Elsayes KM, Emad-Eldin S, Morani AC, Jensen CT: Practical Approach to Adrenal Imaging. Urol Clin North Am 2018, 45(3): 365-387.
- Mao JJ, Dages KN, Suresh M, Bancos I: Presentation, Disease Progression, and Outcomes of Adrenal Gland Metastases. Clin Endocrinol (Oxf) 2020, 93(5): 546-554.
- Da Dalt G, Friziero A, Grego A, Serafini S, Fassina A, Blandamura S, Sperti C: Adrenal metastasis from endometrial cancer: A case report. World J Clin Cases 2019, 7(14): 1844-1849.
- He X, Soleimanpour SA, Clines GA: Adrenal metastasis as the initial diagnosis of synchronous papillary and follicular thyroid cancer. Clin Diabetes Endocrinol 2020, 6(1): 19.
- Washino S, Hirai M, Matsuzaki A, Kobayashi Y: Long-term survival after adrenalectomy for asynchronous metastasis of bladder cancer to the bilateral adrenal glands. Case Rep Urol 2012, 2012: 425230.
- Patel S, Jinjuvadia R, Devara A, Naylor PH, Anees M, Jinjuvadia K, Al-Haddad M: Performance characteristics of EUS-FNA biopsy for adrenal lesions: A meta-analysis. Endoscopic Ultrasound 2019, 8(3): 180-187.
- Sharma KV, Venkatesan AM, Swerdlow D, DaSilva D, Beck A, Jain N, Wood BJ: Image-guided adrenal and renal biopsy. Tech Vasc Interv Radiol 2010, 13(2): 100-109.
- Teegen EM, Mogl MT, Pratschke J, Rayes N: Adrenal Metastasis of Hepatocellular Carcinoma in Patients following Liver Resection or Liver Transplantation: Experience from a Tertiary Referral Center. Int J Surg Oncol 2018, 2018: 4195076.
- Alshahrani MA, Bin Saeedan M, Alkhunaizan T, Aljohani IM, Azzumeea FM: Bilateral adrenal abnormalities: imaging review of different entities. Abdom Radiol (NY) 2018, 44: 154-179.
- Hood MN, Ho VB, Smirniotopoulos JG, Szumowski J: Chemical shift: the artifact and clinical tool revisited. Radiographics 1999, 19(2): 357-371.
- d'Amuri FV, Maestroni U, Pagnini F, Russo U, Melani E, Ziglioli F, Negrini G, Cella S, Cappabianca S, Reginelli A: Magnetic resonance imaging of adrenal gland: state of the art. Gland Surg 2019, 8(Suppl 3): S223-S232.
- Beiderwellen K, Geraldo L, Ruhlmann V, Heusch P, Gomez B, Nensa F, Umutlu L, Lauenstein TC: Accuracy of [18F] FDG PET/MRI for the Detection of Liver Metastases. PLoS One 2015, 10(9): e0137285.
- Farrugia FA, Martikos G, Tzanetis P, Charalampopoulos A, Misiakos E, Zavras N, Sotiropoulos D: Pheochromocytoma, diagnosis and treatment: Review of the literature. Endocr Regul 2017, 51(3): 168-181.
- Martinez M, LeBlanc J, Al-Haddad M, Sherman S, DeWitt J: Role of endoscopic ultrasound fine-needle aspiration evaluating adrenal gland enlargement or mass. World J Nephrol 2014, 3(3): 92-100.
- Mansour KA, Maffei, V, Miller JI, Hatcher CR: Transdiaphragmatic adrenal biopsy. Ann Thorac Surg 1984, 38(1): 66-67.
- O’Malley RL, Godoy G, Kanofsky JA, Taneja SS: The necessity of adrenalectomy at the time of radical nephrectomy: A systematic review. J Urol 2009, 181(5): 2009-2017.
- Repp ML, Alvarez RA, Arevalo-Salzar DE, Kotagiri R: Metastatic renal cell carcinoma and unforeseen adrenal insufficiency: A case report and literature review. Cureus 2023, 15(2): e35265.
Annals of urologic oncology
p-ISSN: 2617-7765, e-ISSN: 2617-7773
 Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.
Copyright © Ann Urol Oncol. This work is licensed under a Creative Commons Attribution-NonCommercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) License.

 Submit Manuscript
Submit Manuscript